Except for Karen Ann Quinlan’s, no other patient’s death has transformed American medical practice so much as that of Libby Zion. Karen Ann Quinlan made history in the mid-1970s when the medical staff at St. Clare’s Hospital in New Jersey would not remove her from a respirator, as her parents wished them to do, even though she was in a “persistent vegetative state.” The Quinlans took the hospital to court and eventually won their lawsuit on appeal; in doing so they helped to define the ethical standards by which the question of when to take someone off life-support systems is now decided. Libby Zion made history in 1984, when she died eight hours after entering New York Hospital’s emergency room with seemingly minor complaints of fever and earache. Her parents, too, took the hospital to court. Even though they did not win their case, they brought into the open the need to reform one of the least well understood aspects of American medicine, its residency training programs.
1.
After years of inquiry into Libby Zion’s death no one can be sure why she died, and who, if anyone, was to blame. A grand jury considered bringing criminal charges against her doctors; the state’s Professional Medical Conduct board held extensive hearings, and a civil court gathered testimony in a trial that lasted several months. To this day no one is certain why an apparently healthy eighteen-year-old suddenly developed a fever that soared to a fatal 108 degrees.
One popularly held theory appeared as Question 49 of the November 1995 pharmacology examination given to second-year students at the Columbia College of Physicians and Surgeons.
Which of the following drugs was administered in the Zion case at New York Hospital and had an interaction with an antidepressant MAO inhibitor that was fatal?
A. Morphine
B. Meperidine
C. Fentanyl
D. Codeine
E. Heroin
The correct answer, according to the examiners, was B, meperidine, more commonly known as Demerol. That answer, however, was wrong. It is true that Libby Zion was taking an anti-depressant, and that the New York Hospital staff should have known better than to give her a sedative like Demerol. But the dose they gave her was very low (in fact, too low to be effective), and there is no case on record of anyone’s dying from the two drugs as administered.
Libby’s parents also got it wrong. Their major claim (among many others) was that the staff physicians were so exhausted from lack of sleep that they could not treat their daughter properly. Not only did they prescribe Demerol incorrectly, but when the nurse on duty reported that Libby was thrashing about, the intern, instead of going to see her, ordered her tied to her bed. In fact, whatever errors were committed were not the result of fatigue. One of the interns was coming off a weekend break and the other had just begun his shift in the emergency room.
New York Hospital also got it wrong. Its lawyers and spokesmen blamed the patient. Had Libby Zion candidly informed the hospital staff about all the drugs she was taking—more precisely, had she told them that she was using cocaine—the outcome, they said, would have been different. But while there was evidence that Libby had taken cocaine shortly before being admitted to the hospital, it was not conclusive. One postmortem analysis revealed a trace of the drug in her nostrils; a second did not. Indeed, the bungling that surrounded the testing of blood and tissue in the Zion case calls to mind the O.J. Simpson case. In both, medical examiners showed a knack for raising more questions than they could resolve.
Even more important, New York Hospital’s effort to shift the blame makes one ask why its doctors had not diagnosed the drug problem themselves. Libby had several textbook symptoms of cocaine use—fever, spastic movements, disorientation—which should have prompted doctors in the emergency room to admit her to intensive care for close observation. But the failure to send Libby to that unit never received the attention it deserved, in or out of court—not the least of the reasons being that the Zions were unwilling to concede that their daughter was likely to have used cocaine. Had they been more open about it, they might have won their case on grounds that even if their daughter had used cocaine, she still should have had the more careful treatment that would have saved her life.
The various legal and medical groups that reviewed the incident did nothing to clarify the cause of death or to ascertain where the ultimate responsibility for it lay. Not only did a grand jury refuse to indict the doctors on criminal charges, but the state Professional Medical Conduct board refused to revoke their licenses. The jury in the civil suit brought by the Zions found fault with both sides. It said that the physicians were negligent in prescribing Demerol and that the intern in charge of Libby Zion was negligent in not following her changing condition more closely and not consulting with senior doctors. But it also found that Libby Zion had taken cocaine soon before her death and had herself been negligent in not providing her doctors with a full and accurate medical history. By blaming everyone, the jury left open the question of whether Demerol, cocaine, incompetence, or viral disease had precipitated Zion’s death.
Advertisement
In her recent book, The Girl Who Died Twice, Natalie Robins is not able to answer the questions that have eluded so many others. A diligent journalist, Robins provides a thorough, if somewhat disjointed, account of a very complex case. She tracked down Libby’s friends, followed the various court hearings assiduously, and spoke to many doctors about medical training in hospitals (although that did not, as we will see, save her from some serious misconceptions about it). Her account moves back and forth between scenes from Libby’s life as she grew up and interviews with the doctors who treated her at New York Hospital. As the book’s title suggests, to understand the death of Libby Zion one must look into the history of both the Zion family and of New York Hospital.
Libby and her father, Sidney Zion, dominate Robins’s account of the family. (She says little about relations between mother and daughter and it is hard to imagine what they were.) Drawing on interviews with Libby’s friends and on their court depositions, Robins depicts Libby as a likable but confused and lonely teenager. She missed many classes in high school and at Bennington College. Her relationships with young men were tangled and unhappy. Like many others of her generation, she used drugs, including cocaine and marijuana. (Her letters, which were introduced as evidence, include passages in which she says that her brain is in a state of “confusion… due to increased amounts of a certain powder entering it.”) And, more than most of her friends, Libby went to doctors. She consulted at least seven, including an internist, a gynecologist, a pediatrician, a psychiatrist, a dentist, and two school physicians; she collected prescriptions to combat stomach trouble, sleeplessness, and depression. Her internist’s chart, which was incomplete, noted that she was taking or had taken Tagamet (for ulcers), Motrin (for pain relief), Actifed (for allergies), Valium and Dalmane (for anxiety), an antibiotic, two anti-inflammatories, an antihistamine, and an antispasmatic; she was also on Nardil, an antidepressant.
Yet her physicians were either unconcerned about or ignorant of the variety of medicines she was taking. Each of them appears to have treated the specific symptoms Libby reported (in person or on the telephone), but paid considerably less attention to the young woman herself. Like many others, Libby knew how to play the medical system, which is so fragmented into mutually exclusive specialties that she had an easy time getting whatever prescription she wanted.
Sidney Zion, a former columnist for The New York Times and later co-owner of a midtown Manhattan steak house, was the main complainant against Libby’s doctors. Robins’s portrait of him is not sympathetic, although she notes that she has known him for over twenty-five years and that he helped with her research. She describes him as aggressive, self-centered, and self-promoting. (Many people have never forgiven him for divulging on a late-night radio talk show that it was Daniel Ellsberg who had leaked the Pentagon Papers to The New York Times.) And, according to Robins, his eulogy at his daughter’s funeral had less to say about her life than about his feelings of indignation at what her doctors had done or failed to do.
Sidney Zion pursued New York Hospital and its doctors with an uncontrolled fury. In his view, they had not committed a regrettable but unavoidable medical error, but outright homicide. “It is my definition of a murder,” he told the state Professional Medical Conduct board. This judgment was malicious and preposterous, but he used it to turn the incident into one of the most effective means for bringing change to American medicine: a scandal.
2.
Although physicians are reluctant to concede it, during the past twenty years the most significant reforms in medicine have been brought about by outsiders. It was mainly lawyers and journalists who helped to stop medical experimentation on human subjects in the US by exposing, among other abuses, the use of unwitting black men for research on syphilis in Alabama and the use of retarded children for research on hepatitis at the Willowbrook State School in New York. It was the relatives of people close to death who forced hospitals and doctors to ask patients whether or not they wished to be kept alive; they supported their case with surreptitiously taken photographs of chalk boards that, unknown to the patients or their families, coded patients on a scale that went from “do everything” to “do nothing.” Patients and their advocates have forced doctors to start giving more accurate accounts of their diagnoses. And women patients helped to change the dominant practice of performing mastectomies in breast cancer cases, allowing women to choose from among far less drastic alternatives. While some doctors were important in introducing these changes, the medical profession left to itself would not have initiated or accomplished any of them.
Advertisement
The training of hospital residents has now also been subject to reform. If not for Sidney Zion’s relentless pursuit of New York Hospital, the unreasonable demands to which hospital residents have been submitted, and their consequences for patients, would have remained unmodified. Several prominent doctors have expressed regret that it took Sidney Zion to reveal the defects of medical training in hospitals. “My wish would be,” conceded Robert Petersdorf, president of the Association of American Medical Colleges, “that the profession had been more perceptive in recognizing the issue and making appropriate changes in training prior to its becoming a cause célèbre.” It was, he said, “unfortunate that long-overdue changes in structuring residency training were not initiated within our own community prior to the serendipitous stimulus of the Zion case.”1 But the profession’s inertia persisted for decades.
Residency training is a wilderness that few non-physicians penetrate. Patients lying sick in a hospital bed rarely inquire of the person with a stethoscope whether he or she is an attending physician, a resident, an intern, or, for that matter, a medical student. (In some institutions, the length of the white coat is the giveaway, but few people know that short jackets identify medical students and knee-length coats “attending physicians,” the senior doctors formally in charge of a patient’s case.) More important, at least until the publicity around the Zion case, almost no one outside medicine appreciated the contradictions inherent in the residency system and their effects on the lives of residents and patients.
These contradictions start with the definition of a resident’s status and tasks. Residents are both advanced students and practitioners: the official term for the three-year resident program is “graduate medical education.” In fact, many teaching hospitals have dropped the labels “intern” and “resident” altogether, using instead the terms Post Graduate Year I, II, and III. Interns are in their first post-graduate year after taking their M.D. degree; residents are in their second and third. As graduate students, residents are expected to read widely in the medical literature and to consult regularly with their putative teachers—that is, the attending physicians. But residents are also practitioners, responsible on a day-to-day basis for diagnosing, treating, and monitoring anywhere from ten to thirty very sick patients. In many hospitals, they are also expected to do “scut work”: drawing blood, inserting intravenous lines, taking specimens to the lab, and so on.
The two roles do not fit together easily either in theory or in practice. Residents are supposed to be supervised as they care for their patients but not supervised too closely. According to the prevailing view, the only way they can learn to practice medicine is by actively making diagnoses, administering drugs, and performing various other medical procedures. If the process is monopolized by an attending physician, the resident’s training will suffer. Accordingly, the guidelines issued by the American Board of Internal Medicine, the certifying body for residency programs, state: “Residents must have continuing responsibility for most of the patients they admit…. Residents must be given the responsibility for decision making and for direct patient care.”2 Supervision is important, but direct experience with patients counts most.
While the official requirements are designed to give residents opportunities to make independent decisions, they have very wide discretion. The result is often what one reform-minded physician has called “resident-run residencies.” Residents usually have primary responsibility over ward patients (that is, poor patients paid for mainly by Medicaid), which gives them an opportunity to learn from treating patients who do not have personal doctors or specialists of their own. Senior physicians provide supervision, but only up to a point—they usually appear on the wards each morning for two hours and make the rounds of patients accompanied by residents and medical students; they may do the same for an hour or two in the afternoon if they are particularly diligent; they are very rarely present at night. For their part, residents on the wards are seldom eager to consult with the senior physicians; they want to work through the case themselves. In most teaching hospitals, to wake a supervisor with a question or to ask him to come to the hospital in the middle of the night would amount to a confession of ineptitude.
This system prompted Michel Foucault to observe that, with the rise of scientific medicine, the poor and the rich struck a Faustian bargain. The poor received treatment on the wards, and in return gave their bodies to the service of medical education. The rich benefited from this knowledge, and in return endowed and supported the hospitals.
But Foucault was only partly right. Residents learn not only by treating the poor but by caring for private patients as well. Even people who endow hospitals or have their own personal doctors or specialists seldom escape the system. All but a few private patients in teaching hospitals go “on service.” That is, they are seen regularly by the resident staff, which writes out their “orders,” including the tests and procedures they are to undergo and the medicine they are to be prescribed. Each patient has an “order book” in which his treatment is entered. It is not, as Robins sometimes suggests, officially closed to attending physicians in the sense that they are prohibited from writing in it; but in practice the orders are entered by the residents, both for “on service” patients as well as for ward patients. Indeed, the American Board of Internal Medicine flatly states: “Residents cannot be expected to show appropriate growth in understanding patient care responsibilities if others write orders for patients under the residents’ care.”
Robins describes both what she calls the “closed” order book—and “on service” care in general. Her discussion is useful in bringing practice in teaching hospitals into the open, but she ignores several critical points. First, the alternative to “on service” care is “off service,” which means that no one apart from nurses and the patient’s private doctor, whose office and home are both likely to be at some distance from the hospital, would be responsible for looking after the patient. (Hospitals usually have a so-called “house doctor,” who is often a moonlighting PGY III; he or she is usually available for emergencies, but little else.) Almost all private doctors put their seriously ill hospitalized patients “on service” so the patient will have around-the-clock scrutiny by the hospital staff, even if it is carried out by young residents.
Second, having residents in control of the order books is not as arbitrary a practice as it might appear. Since they are almost always assigned to a specific hospital floor, they are more likely to keep their eye on the order books of a particular group of patients; they observe the patient from hour to hour if necessary and this reduces the chance of errors arising from orders that are contradictory or should have been revised.
Finally, Robins fails to recognize that the ways doctors work with house staffs on behalf of private patients vary enormously. Many busy practitioners count on the residents to provide care for their patients and would never consider writing in the order books that the residents maintain. Some doctors insist on being called in if their patients begin sneezing; they refuse to give residents any leeway in making decisions and will take over the order book if the resident is not immediately on hand. Residents quickly learn each attending physician’s style; naturally they prefer the one who gives them the most latitude. The “closed” order book is not “the dirtiest little secret in medical education,” as Robins puts it, but, whether for reasons of ego or embarrassment, physicians generally fail to explain to patients how much of their treatment will be in the hands of residents.
Before Libby Zion’s death her family had little idea how a hospital worked. They assumed, for example, that since their doctor had sent Libby to the emergency room at New York Hospital, he would be in charge and on the scene. But the case was handled in the usual way—that is, Libby was put “on service.” In fact, the residents called and spoke to the attending physician several times. No record exists of these conversations, but it seems most unlikely from the evidence that the residents told him, or implied, that he should come to the hospital. Neither the admitting diagnosis (“viral syndrome with hysterical symptoms”) nor the admitting orders (to merely monitor the patient’s vital signs) suggested that Libby’s condition was critical. When a nurse asked an intern to see the increasingly agitated patient, the intern treated her request casually, as if there was no cause for intense concern. In those circumstances few private physicians would have gone to the hospital; most of them would have done so only if they had an urgent call from the house staff or if they had a special relationship with the patient.
Would a more experienced doctor have sent Libby to the intensive care unit? Should not the intern have come to see Libby as her fever rose? In hind-sight most of the physicians I know would say yes to both questions, but there is no way to be sure what should have been done at the time. All that can be said is that no senior physician on the hospital staff ever examined Libby. Neither New York Hospital nor most of the other hospitals I know of kept a senior doctor on hand to review decisions made by emergency room residents. That they should now do so was one of the two major proposals for reform that were provoked by Libby Zion’s death.
The second reform concerned how long residents work. Until the Zion case, it was commonplace for residents to be on the job 100 to 120 hours per week and to be on call every third or fourth night (during the 1930s and 1940s, they were on call every second night). Once or twice a week, each resident worked a thirty-six hour shift (from 7 AM the first day through 7 PM the second day, returning the next morning at 7 AM). The most obvious result was that residents did almost anything to cut down on their night-time tasks simply to get some sleep. A harrowing account of their working lives was given in 1986 by the sociologist Terry Mizrahi in her book Getting Rid of Patients, which described the variety of strategies residents used to avoid a “hit” (their term for a patient admission) or, failing that, to ease their workload. But so far as I know Mizrahi’s book had no effect on medical training.
Although virtually everyone in charge of medical schools and hospitals recognized the drawbacks of a 120-hour week, they not only accepted the arrangement but strongly defended it. Since patients needed “continuity of care,” so the argument went, it was better to have a tired doctor who knew the case than a rested one who had only read the chart. Critical illnesses, it was said, often develop over several twelve-hour periods; so shorter hours would mean that residents would miss a vital training experience. Most important, residents had to learn that medicine was a calling, not a job, and that one’s responsibility to one’s patients took precedence over all other considerations, including sleep. Put residents on a fixed schedule and they would come to adopt a lax “shift mentality.”
None of these propositions, however, was ever actually tested. In a profession that prides itself on rigorous trials for every new drug and procedure, few hospital directors experimented with different schedules or examined charts to see if the theory of twelve-hour periods had any bearing on how illnesses really developed. No one challenged the idea that sleeplessness instilled a professional ethos in interns or wondered why learning how to avoid seeing patients was so important a part of a young physician’s education. When the occasional critic noted that, apart from those in military service in wartime (and, some would add, new mothers or writers and editors facing deadlines), no one else regularly worked under conditions of sleep deprivation, the medical community insisted that a different system would be worse by far.
Ironically, as I have mentioned, the residents who treated Libby had not lost sleep. But once the facts of residency training came into the open, demands for change became inevitable. To the grand jury that reviewed the Libby Zion case, it seemed obvious that if the Federal Aviation Association said that pilots had to have “nine consecutive hours of rest for less than eight hours of scheduled flight time,” residents should not be treating patients for thirty-six hours straight. The grand jury also found that interns were not adequately supervised and recommended that hospitals change the prevailing arrangements for overseeing their work.
In response, David Axelrod, then head of the New York State Department of Health, appointed a commission chaired by Professor Bertram Bell of the Albert Einstein College of Medicine in 1986. After numerous hearings and over strenuous objections from doctors, the Bell Commission recommended several major reforms which were officially adopted in 1989 as Section 405 of the New York State Health Code. The work week of medical interns cannot exceed an average of eighty hours; they are not to work more than twenty-four consecutive hours and must have one twenty-four-hour period free each week. Every hospital emergency room has to have an attending physician present and on duty, and every hospital has to have an attending physician on call should residents require a consultation. The state provided hospitals with additional funds to defray the added costs of these reforms, including payments to auxiliary workers to do “scut work” and an increase of about 10 percent in the number of residency slots.
3.
New York’s precedent has transformed residency training throughout the country. Although no other state has issued similarly specific regulations, practically every group that accredits residency programs now insists on a less crushing schedule (except in training for surgery, which has successfully resisted all pressures). The new requirements for residents in internal medicine, for example, are that they should spend, on average, no more than eighty hours a week in patient care; that they should be on call no more than one night out of three; and that they should have one day a week free. The administrators of hospital residency programs have adopted similar provisions—perhaps because they agree that they are necessary, but more likely because they must remain competitive with other programs. Had they not modified their demands, New York hospitals would have enjoyed a huge recruiting advantage over hospitals in other states.
The general consensus about the need to change residency programs has not produced any clear agreement on the value of the changes that have so far been made. As might be expected, the residents themselves are overwhelmingly in favor of them. Although the letter of the law is frequently violated (the hour limits are neither consistently followed nor enforced), workloads are generally lighter. Residents in internal medicine at Albert Einstein College of Medicine told researchers that “the regulations had reduced their fatigue on the wards and lessened emotional stress…. They now provided better patient care.”3 Residents in obstetrics and gynecology at the Columbia-Presbyterian Medical Center said that, with no diminution in the quality of patient care, there was “a marked improvement in the quality of their personal lives, the amount of sleep they achieved, and their level of stress.”4 Even surgical residents are convinced that “long consecutive hours impair quality of patient care.”5
On the other hand, senior physicians complain bitterly that residents have, as they had feared, adopted a shift mentality and that patient care has suffered. Residents, they say, leave tests uncompleted and ignore anyone who challenges them when they head for home. Most residents deny the charge, maintaining that they are not clock watchers and have not lost their sense of professional responsibility. Most attending physicians say they do not believe them.
Only one study has attempted to measure by objective standards the effects of the new rules on patient care. At New York Hospital, of all places, investigators reviewed patients’ charts immediately before and after the changes; they found that the new system increased delays in obtaining test results. The study also measured the changes in “in-hospital complications,” which include ignoring abnormal test results and making errors in prescriptions and dosage. It found no change had occurred in the total number of tests performed, the length of time patients spent in the hospital, the number of transfers to intensive care, or, most important, mortality rates.6 But the study has its weaknesses—the category of “in-hospital complication” is very loosely defined—and its findings might not hold true for other hospitals.
Whatever further investigations may show, there is no going back to the 120-hour workweek, in part because the public and the medical residents will not tolerate it, and in part, too, because residency in the 1990s, even after these changes, is a far more demanding and stressful experience than it was twenty years ago. Contrary to previous practice, Medicare and HMO regulations require that only people with very serious illness be admitted to a hospital. Patients also remain in hospitals for much shorter periods, from an average of twelve days in the early 1980s to under eight days now, owing to new and more complex technology for diagnosis and treatment as well as to constantly rising costs. It was one thing to work thirty-six hours when residents only had to read an EKG or listen to a stethoscope. It is quite another when they may be prescribing fast-acting cardiac drugs or performing more intricate and invasive diagnostic procedures, such as inserting a catheter into the heart to measure its output of blood.
In any case, the private doctor, who acted both as an entrepreneur and as a heroic figure to his patients, is giving way to the team member who is part of an HMO or a physician-run practice plan, an interchangeable part of a larger medical system. More and more he is forced by the schedules and rules of group practice to hand off a patient to colleagues and to try to do so in a way that ensures continuity of treatment. The once traditional question “Who is your doctor?” is changing to “Which health care plan do you belong to?” How many people now in their twenties are likely to develop a close personal relation with, and loyalty to, one particular doctor? In view of the direction in which the medical system seems to be heading, a carefully designed system of shifts may be precisely what doctors require.
Changes in medicine are beginning to mirror the “restructuring” that is taking place within other organizations. The doctor-patient relationship is increasingly formal and bureaucratic; more and more it is an exchange between strangers based on increasingly sophisticated methods of testing and treatment. In many cases medical practice has become more efficient, but it may also leave some patients feeling stranded, without the intimate observation of their symptoms and the sympathetic advice they formerly expected. This new situation is not what Sidney Zion had in mind when he began his campaign; but it may help to explain the degree to which he succeeded in changing the way doctors work in America.
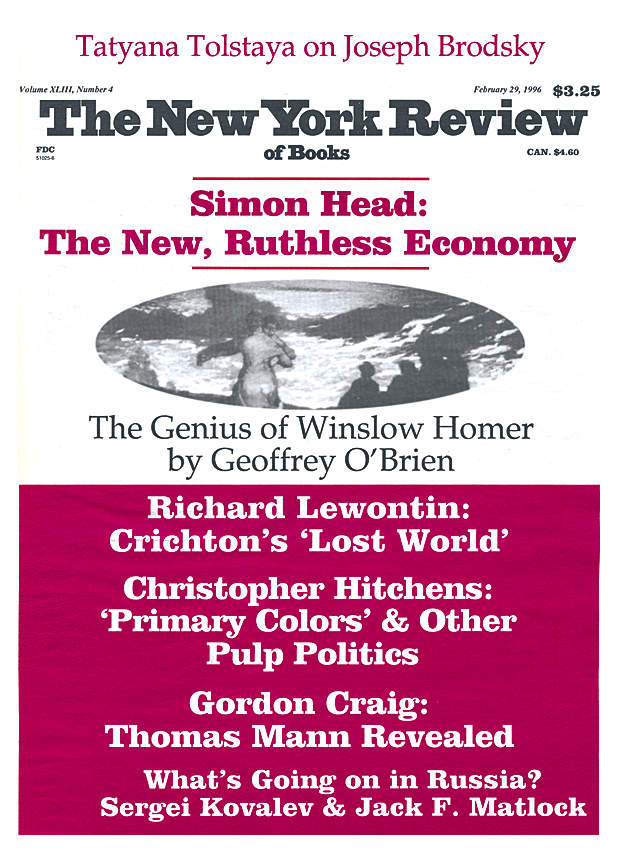
This Issue
February 29, 1996
-
1
Robert G. Petersdorf, M.D., “Regulation of Residency Training,” Bulletin of the New York Academy of Medicine, July-August 1991, p. 330. ↩
-
2
Graduate Medical Education Directory, 1995, pp. 62–63. ↩
-
3
Joseph Conigliaro, William Frishman, Eliot Lazar, and Lila Croen, “Internal Medicine Housestaff and…the Impact of New York State Section 405 Regulations…,” Journal of General Internal Medicine, 8 (1993), p. 505. ↩
-
4
Amalia Kelly, Frances Marks, Carolyn Westhoff, and Mortimer Rosen, “The Effect of the New York State Restrictions on Resident Work Hours,” Obstetrics and Gynecology, 78 (1991), p. 468. ↩
-
5
Steven Ruby, Lisa Allen, Peter Fielding, and Peter Deckers, “Survey of Residents’ Attitudes Toward Reform of Work Hours,” Archives of Surgery, 125 (1990), p. 765. ↩
-
6
Christine Laine, Lee Goldman, Jane Soukup and Joseph Hayes, “The Impact of a Regulation Restricting Medical House Staff Working Hours on the Quality of Patient Care,” Journal of the American Medical Association, 269 (1993), pp. 374–378. ↩