To the Editors:
My colleagues and I at the World Bank commend The New York Review for its continued thought-provoking coverage of the HIV/AIDS crisis. Unlike the many writers who have attempted to reduce the entire issue to a single dimension (e.g., abstinence, drugs, money), Helen Epstein captures the challenge of the pandemic in its full, formidable complexity.
We particularly welcome her emphasis on the centrality of community-based organizations [“AIDS in South Africa: The Invisible Cure,” NYR, July 17]. Community norms are among the most powerful determinants of individual behavior, and thus pivotal to effective HIV prevention. Grass-roots organizations are also the leading providers of AIDS care and support. Thousands of these “social antibodies” have sprung up in the past decade to fight the epidemic, and in the process pioneered many of the most effective programs yet devised. For the poorest and most marginalized groups, they are often the only source of support or services.
For this reason, we would like to correct one error in the article. Ms. Epstein worries that major donors will overlook community-based groups in favor of costly mega-projects. The World Bank, however, supports grassroots NGOs and other groups as a cornerstone of our $1 billion Multi-Country HIV/ AIDS (MAP) Program for Africa. Roughly half the resources under the MAP are expressly reserved for these groups and managed through fast, simple mechanisms.
In countries across Africa, the MAP has already funded thousands of community and NGO micro-projects in amounts averaging only a few thousand dollars each. In many cases, this represents the first time such groups have ever received public funding, allowing them to sustain or expand their activities. The Bank is committed to helping such groups succeed in their vital role.
Keith Hansen
Manager, AIDS Campaign Team for Africa
The World Bank
Washington, D.C.
To the Editors:
Helen Epstein suggests that a cure for South Africa’s AIDS epidemic might be in a cultural revolution to break the code of silence about AIDS among black South Africans allowing people to acknowledge the disease and its devastating consequences for their lives. Openness in communicating personal experiences about the suffering of AIDS would lead to greater compassion toward those already afflicted and to a decline in new infections. Instead, South Africa has paradoxically—given Mr. Mbeki’s search for a uniquely “African” solution to an African tragedy1—embraced a crassly Western, consumer-oriented program (the loveLife project) that promotes assertiveness, choice, empowerment, and positive approaches to safe sex, while skirting the depressing details of the epidemic which might alienate adolescents.
Both approaches, however, focus on individual behaviors when the root causes of the South African epidemic lie in the legacy of apartheid’s barely concealed genocidal project. As Epstein has written in an ear-lier article, the mad social engineers of apartheid forced male workers to live in worker hostels that destroyed the social fabric of proudly patriarchal peoples.2 Contained to concentration camp–type barracks near mines and factories, workers took temporary “wives” and formed “bedholds” in place of households.3 When women were unavailable to service the army of displaced workers recruited from all over southern Africa, migrant workers engaged in same-sex relations, violating strong cultural taboos. Out of this crucible of forced migration, family disruption, inhumane living conditions, and general human misery was born an environment ripe for a sexually transmitted epidemic.
Frank talk about sex, death, and human suffering in the time of AIDS is a good thing, but it won’t “cure” the epidemic. By the time most people anywhere in the world realize what AIDS is doing to them—i.e., when those close to them start dying—the damage with respect to transmission is already done.
The real problem of AIDS denial, as Epstein previously noted,4 lies outside South Africa’s impoverished townships. The state itself is in denial. While NGOs can prod governments into action, they cannot take their place. Epidemics require strong medical and public health institutions, providing early and coherent prevention and adequate medical care.5 Thus far, most South Africans are receiving neither.
While, as Epstein notes, antiretrovirals are not a cure for AIDS, they do prolong life. South Africans deserve the same medical citizenship as AIDS patients in the US, Europe, and Brazil. They cannot be told to go home and face death quietly. Treated, AIDS patients return to work and to the care of their young ones. Untreated, they leave behind orphans and a decimated workforce. When dying people are restored to health before the eyes of the community, the ambiguity, myths, and denial about the viral cause of AIDS deaths are put to rest and treatment becomes the best educational tool available.
South Africa’s Constitutional Court has just ruled that the government’s current AIDS policy is an infringement on the constitutional “right to health care.”6 On August 8, 2003, President Mbeki’s administration finally committed itself to developing a national HIV treatment plan, an about-face that could result in 1.2 million people receiving generic antiretrovirals within five years.7
But even generic drugs are prohibitively expensive.8 With 80 percent of South Africa’s population dependent on the state for health care, the current per capita expenditure is only $85.9 So where is the money to come from? Given its root causes, South African AIDS patients deserve a share in any reparations paid to the victims of gross human rights abuses. Wole Soyinka’s proposal10 of a “reparations tax” levied on all white South Africans who were the beneficiaries of apartheid’s violence could be extended to all nations that benefited from South Africa’s forced labor policies. The global economy contributed to the spread of AIDS. Now it’s time for a “global society”11 to pay its dues.
Nancy Scheper-Hughes
Professor of Medical Anthropology
University of California
Berkeley, California
Helen Epstein replies:
I welcome Mr. Hansen’s correction.
Nancy Scheper-Hughes criticizes my proposal, as well as the loveLife program, because, she says, both emphasize “individual behaviors when the root causes of the South African epidemic lie in the legacy of apartheid’s barely concealed genocidal project.” I am not sure what she means. Is not sexual intercourse, whatever its “root causes,” a behavior carried out by individuals? In any case, the primary difference between the approach I advocate and loveLife’s is that while loveLife aims to persuade young people that avoiding HIV is in their own individual self-interest, the approach I advocate aims to encourage greater communication about the reality of AIDS among groups of people, and even entire communities. The two approaches could not be more different.
The only model for past successful HIV prevention that Scheper-Hughes provides in her letter is Cuba in the 1980s. At the time, HIV was largely limited to homosexuals and Cuban soldiers returning from Africa, who were tested for HIV and quarantined. They are believed to have received excellent health care by Cuban standards, but they were not allowed out of quarantine on their own unless the authorities were confident that they could be trusted not to infect others. I find it hard to believe that Scheper-Hughes is suggesting that the South African government quarantine all five million of its HIV-positive citizens. Not only would the HIV prevention methods employed in Cuba be unpopular in Africa, they would also be far more expensive than any of the already underfunded treatment or prevention programs proposed or underway.
In fact, Scheper-Hughes goes on to suggest something quite different for South Africa. In her view, the only way to prevent further spread of HIV in South Africa is to give antiretrovirial drugs to everyone with AIDS. While I very much hope that the government of South Africa will live up to its recent promise to do this, there is as yet little evidence that antiretroviral treatment programs run by governments automatically lead to reduced HIV infection rates on their own. Since the introduction of nearly universal HIV treatment in the US in 1996–1997, the annual number of new infections has increased, and the drugs themselves have been at the center of much of the “ambiguity, myths and denial” that Scheper-Hughes maintains should have gone away.
In addition, the Botswana government has one of the most comprehensive government-run AIDS prevention programs in Africa, and it launched an HIV treatment program two years ago that is a model for the rest of the world. Despite this extraordinary effort, the most recent survey shows the virus is still spreading at the same, staggering rate, so that Botswana has the highest infection rate of any country on earth. I trust that HIV rates in Botswana will eventually fall, and the faster they do, the more lives will be saved. But it is worth asking why it is taking so long.
In African countries where HIV is widespread in the general population, and where HIV rates have subsequently declined, the involvement of civil society seems to have been a crucial factor. HIV rates in Uganda and Kagera, Tanzania, fell 70 percent between the late 1980s and the present, when medical care was abysmal and virtually no one received antiretro-viral treatment in either place. While the government response to the epidemic in Uganda was vigorous, the government response in Tanzania was desultory, as was the response in Zambia, where HIV rates have also fallen, although more slowly. HIV rates among gay men in the US fell by 70 percent beginning in the early 1980s, when there was no treatment at all for AIDS, and the US government was extremely indifferent to the plight of these men, providing very little funding for prevention or care.
It will be some time before the anti-retroviral program Scheper-Hughes envisions is truly universal, even in South Africa, which has the money to pay for these drugs. It will probably take far longer for these drugs to reach most people with AIDS in other, poorer African countries. In the meantime, Scheper-Hughes’s apparent objection to HIV prevention programs is unfortunate in view of the fact that they have saved thousands, if not millions, of lives in other countries.
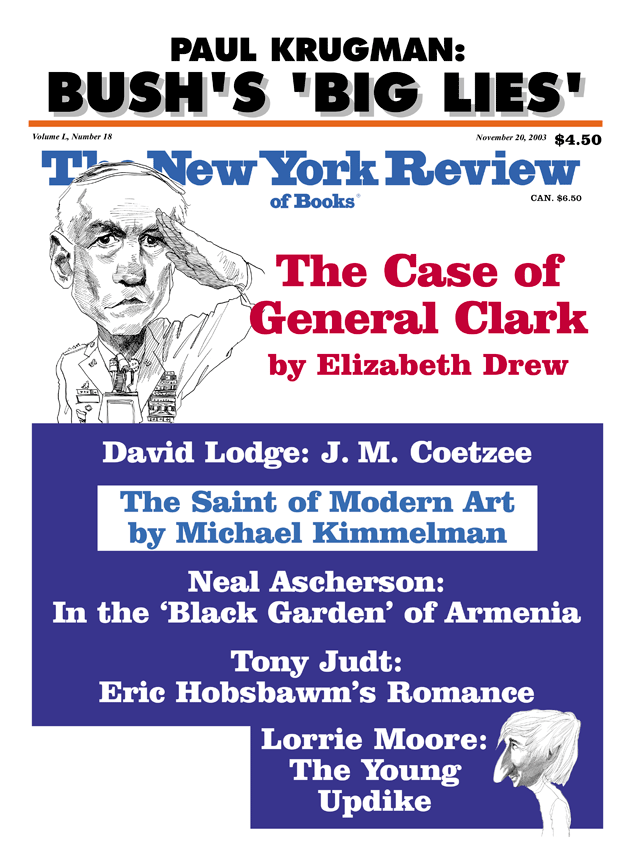
This Issue
November 20, 2003
-
1
Mbeki has argued, with reason, that AIDS in Africa is a “uniquely African catastrophe.” But foremost among the differences (for Mr. Mbeki) is the “heterosexual mode of transmission” in South Africa, which is in itself a denial of the fluidity of sexual relations necessitated by the history of labor migration under apartheid. (See Mbeki’s open letter to world leaders, April 3, 2000, www.sumeria.net/aids/mbekiltr.html.) ↩
-
2
See Helen Epstein, “The Hidden Cause of AIDS,” The New York Review, May 9, 2002. ↩
-
3
See Mamphele Ramphele, A Bed Called Home: Life in the Migrant Labour Hostels of Cape Town (Ohio University Press, 1993). ↩
-
4
Helen Epstein, “The Mystery of AIDS in South Africa,” The New York Review, July 20, 2000. ↩
-
5
Cuba’s successful national program of public health surveillance and treatment sanatoria, pursued in the face of accusations of human rights violations of personal liberty and privacy, is a case in point. See Sheri Fink, “Cuba’s Energetic AIDS Doctor,” American Journal of Public Health, Vol. 93, No. 5 (May 2003), pp. 712–716; also Nancy Scheper-Hughes, “AIDS and Human Rights in Cuba,” The Lancet, Vol. 342, pp. 965–967. ↩
-
6
See George Annas, “The Right to Health and the Nevirapine Case in South Africa,” New England Journal of Medicine, Vol. 348, No. 8 (February 20, 2003). ↩
-
7
See Anne-Christine d’Adesky, “HIV Generics: Ready for a Revolution?” American Foundation for AIDS Research (August 2003). ↩
-
8
The annual cost in Brazil in 2000 was $4,292 per patient. ↩
-
9
Solomon R. Benataur, “South Africa’s Transition in a Globalizing World: HIV/ AIDS as a Window and a Mirror,” International Affairs, Vol. 77, No. 2, pp. 347–375. ↩
-
10
See Wole Soyinka, The Burden of Memory: The Muse of Foreignness (Oxford University Press, 1998). ↩
-
11
See George Soros, “Toward a Global Open Society,” The Atlantic Monthly, January 1998, pp. 20–32. ↩