Speak, Memory, Vladimir Nabokov called his book about his childhood years, and in this incantatory title we can hear our human dread of forgetting. “The cradle rocks above an abyss, and common sense tells us that our existence is but a brief crack of light between two eternities of darkness,” reads the book’s first sentence. The crack of light may be described as memory itself—that fickle and unreplicable network of experience and associations from which we construct who we are, who others are, and what we may expect from them and from ourselves.
In the broadest sense, memory is consciousness, because what the brain is doing at all times and in all of its operations is remembering. More often than not, it is a matter of practical cognition: knowing where we left the keys, and then, once we have located them, what the keys are for. But within such memories are vestiges of our emotional and sensorial lives, an intimate network of recollections, unique to each of us, that keys conjure. The neurosystem in which this cascade of memory occurs, with its branches and transmitters and ingeniously spanned gaps, has an improvised quality that seems to mirror the unpredictability of thought itself. It is an ephemeral place that changes as our experience changes, to the point where we are incapable of remembering the same event in exactly the same way twice.
In her fascinating book about memory loss and the efforts of scientists to understand it, Sue Halpern reports an experiment in which members of the Cambridge Psychological Society were asked to reconstruct a meeting of the society that had taken place two weeks before. The average person was barely able to recall 8 percent of what had happened, and almost half of this was incorrect, peppered with the recollection of events that had never occurred or that had occurred elsewhere.
Such paltry power of retrieval in an educated, and supposedly attentive, group is not surprising. Memory, Halpern reminds us, “is not an archive,” nor does it record in real time. It lives in the brain “in chemical traces. The traces can fade…and they can be augmented,” depending on one’s experience and observation. The intensity of an experience may sharpen the memory of it, while making it even less accurate. During situations of extreme stress, for example, the body is flooded with damaging amounts of the hormone cortisol, causing communication relayed by neurotransmitters and other chemicals in the brain to break down. Halpern recounts the case of an Australian forensics expert named Donald Thomson who was a guest on a television show devoted to exploring the unreliability of eyewitness testimony:
Not long afterward [Thomson] was summoned to a police precinct, put in a lineup, and identified by a woman as the man who had raped her. Though he had an incontrovertible alibi—he was on national television at the time of the attack and seen by hundreds of thousands of viewers—he was charged with the crime on the basis of her unwavering eyewitness testimony. It was only later, when an investigator discovered that the woman’s television had been on during the assault, that it became clear that in the midst of her trauma, the woman had conflated Thomson’s face with that of the rapist.
In spite its unreliability, however, our memory is the fullest record we have of ourselves. We live through it as we live through breathing, and not only in the figurative sense: in the most advanced stage of Alzheimer’s—a disease that first strikes the hippocampus, where short-term memory is created, before spreading throughout the rest of the brain—one forgets, on a muscular level, how to exhale.
Halpern’s central aim in Can’t Remember What I Forgot is to find out how memory loss occurs, when it ceases to be a normal condition of aging and becomes a disease, and what the prospects are for the development of a drug that can stave it off. Playfully, she frames her investigation as a quest for esoteric knowledge: skeptical, open-minded, and omnivorously curious, she goes where the rest of us cannot go, penetrating the inner sanctums of America’s memory research labs to bring back the news. She twice submits herself to injections of radioactive material in order to get up-to-the-minute functional images of her brain; undergoes hours of paper-and-pencil neuropsych exams that put her memory and spatial reasoning to the test; takes a cognitive stress test (in which the brain takes in new information, encodes it, and retrieves it, while the MRI takes “pictures that show which parts of the brain are being activated, which parts are working harder than normal”); attends memory-boosting seminars; and at home practices a variety of mental exercises designed to sharpen her cognitive prowess.
Advertisement
In San Francisco, Halpern sits in on a “brain-fitness class.” And in Manhattan she witnesses a one-on-one session at a psychologist’s office, where
a fellow in his forties who wanted to “stay sharp” was coached through a series of mental stretching exercises adapted from a rehabilitation regimen originally designed for stroke victims and people with traumatic brain injuries. There was nothing particularly wrong with him, he said, but he was now single, after years of marriage, and he was hopeful that a tuned-up memory would give him an edge in the dating game.
At one point, at UCLA’s Brain Mapping Center, Halpern has her hippocampus “unfolded,” using magnetic resonance imaging and math, in order to measure the thickness of each of its six cortical layers. The thicker each layer is, the healthier, since Alzheimer’s begins with a thinning of the hippocampus’s entorhinal cortex—an important memory center in the brain—as a result of the death of neurons there. (In non-Alzheimer’s memory loss a different node of the hippocampus is affected, the dentate gyrus.) When neurons in the entorhinal cortex fail to project into the next region of the brain, the neurons in that region die as well, starved of the connections needed to keep them alive. Recent recordings taken from the brains of epilepsy patients show that specific spontaneous memories are stored in specific neurons in the hippocampus.1 As those neurons fail to ignite, the capacity for free recall diminishes until it is wiped out entirely. The loss is sequential. “This may be a fifty-year process,” Dr. Susan Bookheimer of the Brain Mapping Center tells Halpern. “It’s a long process that will spread and spread.”
In all of the tests, Halpern’s brain performs well, but this fails to assuage her anxiety about the future. She knows that early detection of Alzheimer’s is difficult, and that, as with many types of cancer, by the time impairment is diagnosable it’s too late. Moreover, early detection comes with psychological peril, since there is no treatment capable of warding off dementia’s later stages. Most people reasonably prefer ignorance to certainty when given the choice of knowing whether they will get a disease with no cure. Halpern writes that when signs of Alzheimer’s show,
this is when you begin to say that someone is not herself. We even say this about ourselves. But how can that be?… How can you be anything but yourself? The obvious, rational answer [is] that you can’t…. You are only yourself now. And what if that self is one who can’t remember itself? What if the person you had been is only a memory…held by others?
These questions go to the heart of our anxiety about memory loss. According to a survey conducted by the MetLife Foundation, in 2006, Americans over the age of fifty-five fear getting Alzheimer’s more than any disease. (Among respondents of all ages, Alzheimer’s was second only to cancer.) Near the beginning of Can’t Remember What I Forgot, Halpern gives a brief description of her father’s mild cognitive impairment (MCI). He is in his mid-seventies, and he knows how disorienting it is “to pick up the phone to call a friend, whose funeral he’d attended two years earlier.”
During the year before his death he would often sit at “the kitchen table from breakfast till lunch staring at a single page of the New York Times.” Halpern’s mother has bought him a key-chain recorder with his name and address in case he gets lost, but he dies before having to use it. The doctor has assured Halpern that he did not have Alzheimer’s, but he never underwent an autopsy that would have shown unequivocally whether the gummy mess of beta-amyloid plaques that is the telltale symptom of Alzheimer’s had infected his brain.
Not everyone with MCI goes on to develop Alzheimer’s, and some people diagnosed with MCI turn out not to be impaired. Comparing people with MCI at the time of diagnosis and two years later, Susan De Santi, a psychologist at NYU’s Center for Brain Health, found that some actually went back to being normal. For the most part, these people were younger and more educated than the group as a whole, suggesting that, through various means of intellectual and physical stimulation, they had developed alternative neural pathways that allowed them to make up for weaknesses in other parts of their brains. It was a kind of cognitive reserve. De Santi tells Halpern in a “quiet and conspiratorial” voice:
People think that MCI is only about memory, and in fact, only those who converted to AD had significant declines in memory. But we also found that it’s not memory alone. It’s memory problems combined with problems in some other cognitive domain, like fluency or spatial reasoning. Seventy-one percent of those who had memory problems and some other problem ended up getting sick with AD, but only eight percent of people who only had memory problems got sick…. For people who went back to normal, the significant thing was that they had no attention deficits. Attention, not memory, was really the key.
But of what comfort is all of this diagnostic wisdom in the face of a disease that strikes, with alarming frequency, a growing population of elderly people whether they are educated or not?2 John Bayley, in Elegy for Iris, his memoir of his marriage to the novelist Iris Murdoch, who suffered from Alzheimer’s during the last years of her life, likens her mental state to that of one condemned to collect water with a sieve. Language is one of the first faculties to break down. Their mode of communication, Bayley writes, “seems like underwater sonar, each bouncing pulsations off the other, then listening for an echo.” Even when words come, they are not accompanied by “that wordless communication which depends on the ability to use words.”
Advertisement
A particularly diabolical feature of Alzheimer’s is that, while all else has washed away, “emotional memory” is retained, so that the patient finds himself in a prison of feeling without context. A friend has told me of his normally mild-mannered father who, enraged at being unable to figure out how to insert his key into his locked car, hacked the door off with an axe that he kept for splitting firewood. He began eating soap, toilet paper, and worse—extreme behavior, but not untypical. To tamp down his delusions, he was given haloperidol, an antipsychotic medication that blocks the manufacturing of dopamine in the brain, thereby accelerating his cognitive decline.
The 36-Hour Day, an admirably realistic guide to caring for people with Alzheimer’s, warns of the patient’s occasional “catastrophic reaction”: tantrums, violent resistance, cursing, and intense panic in response to the demands of simple tasks, such as taking a bath or undressing or going out for a walk. On the opposite end of the spectrum is a clinging docility, distress when the caregiver is out of sight even for a minute, and what clinicians call “the lion’s face” of Alzheimer’s patients, an impassive mask that transmits nothing so much as its owner’s living absence. The authors of The 36-Hour Day offer caregivers trying to cope with this predicament a series of grimly gentle admonishments:
Be patient…. Remember, the person you are caring for often is also miserable and is doing the best he can…. Do not make assumptions about what he understands…. He’s not doing these things to hurt you….
Occasionally a person with a dementing illness will insist that her spouse is not her spouse or that her home is not her real home….
Reassure the person, “I am your husband,” but avoid arguing. Although this may seem heartbreaking, it is important for you to reassure yourself that it is not a rejection of you (the person does remember you). It is just an inexplicable confusion of the damaged brain.3
A drug capable of curing such a disease would bring incalculable benefits. It would also be enormously profitable, since atrophy of the hippocampus occurs in schizophrenia and other psychiatric disorders as well as in normal aging —a potentially limitless market. Halpern’s description of the competition to develop a so-called “smart drug” is knowing and trenchant. Almost every time she questions a scientist with a memory drug in development, she is told that it will be on the market in “five years,” which in pharmaceutical-speak translates as “maybe never.” A highly secretive start-up company that boasted as one of its lead researchers the 1972 Nobel laureate for physics, Leon Cooper, claimed to have “an honest-to-God gold mine of a wonder drug” that turned out to be a derivative of amphetamine.
More likely candidates for success seemed to be drugs in development at Memory Pharmaceuticals, co-founded by Eric Kandel. Kandel was awarded the Nobel Prize in medicine in 2000 for his seminal observation that it was in the action of the synapses between cells that memory existed, not in the cells themselves, and that a molecule called cyclic AMP was what allowed cells to retain memory over the long term.4 Influenced by Kandel’s findings that inhibiting the breakdown of cyclic AMP improved the function of the hippocampus of aged mice and their memory performance, scientists at Memory Pharmaceuticals developed new compounds that inhibit the breakdown of cyclic AMP. ��The company is now in Phase II clinical trials with these drugs.
In high doses the drugs appear to have had a detrimental effect on the prefrontal cortex of monkeys, exposing, in Halpern’s words, “the limits of relying on reductionist science when making the leap from describing molecular pathways to manipulating them.” Many other promising smart drugs have fizzled, including a highly touted attempt by Elan Pharmaceuticals to create a vaccine against the buildup of toxic amyloid plaques. Just this past July, another beta-amyloid inhibitor called Flurizan, similar in its structure to the pain reliever ibuprofen, was abandoned by the biotech company Myriad Genetics after being the first drug of its kind to reach late-stage testing.
Disappointments such as these are to be expected in the natural course of scientific research; the chances of any compound making it all the way through clinical trials and FDA approval—at an average price of $500 million—are about five thousand to one. For drugs that target the brain the odds are even longer. First, there is the problem of getting past the blood-brain barrier, a protective sheathing designed to keep foreign matter out of the brain tissue. Systemic delivery of a compound, via the bloodstream, can cause dangerous side effects. Beta-amyloid, for example, is produced throughout the body, and blocking it in areas of the body other than the hippocampus can weaken the immune system. Even if a reliable mode of delivery can be found, there is still the question of precisely where to aim a drug. Halpern puts it succinctly: “memory…resides throughout the brain, it is by design a moving target.”
In recent years, researchers have come to realize that amyloid plaques are a secondary result of Alzheimer’s, not the cause. The source of the disease is somewhere further upstream. But where? In a specific gene? In the neurotransmitters that make the synapses fire? A persistent, and not irrational, hope is that the key to the process by which neurons are created—neurogenesis—lies within some ordinary, ubiquitous compound that is staring us in the eye, such as blueberries, beta- carotene, omega-3 fish oil, gingko biloba, almonds, nicotine, estrogen, flavanol-rich green tea or cocoa or red wine, to name several suspects. None has panned out so far, but to cover their bases a few of the country’s leading neuroscientists have filed patent applications for seemingly unpatentable food-types, or at least for the correlation between them: blueberries + fish oil + Merlot, to give a plausible example.
Predictably, the anxiety surrounding memory loss has spawned a multibillion-dollar industry of over-the-counter nutritional supplements and “cognitive enhancers.” Memory improvement is a rising fad, as demonstrated by the success of “Procera AVH,” a vaguely defined “cognitive restorer” in pill form that is the brainchild of John Reynolds, inventor of the thighmaster and the mood ring. The number of books promising “superpower memory,” “eternal brain youth,” and, in one case, liberation from the “myth of Alzheimer’s disease” is rivaled only by diet books. Nintendo Brain Age is one of several digital gaming devices marketed to the nervously healthy middle-aged.
If Can’t Remember What I Forgot can be said to have a hero, it is the neurologist Scott Small, whom Halpern regularly debriefs at his office at Columbia University’s Neurological Institute. Unlike most neuroscientists, who focus on known pathologies, Small studies normal memory decline. In Halpern’s portrayal, he possesses a highly original intelligence, plenty of horse sense, and an endurance for the ploddingly incremental tempo of progress that makes brain science a gamble comparable to that of spending half a lifetime writing a novel. Small did not discover that Alzheimer’s disease first strikes the entorhinal cortex. He discovered that age related memory loss is distinct from Alzheimer’s disease in having its onset in the dendate gyrus.
One of his aims is for entorhinal cortex dysfunction to replace amyloid plaques as the “diagnostic gold standard” for Alzheimer’s. He believes that the key to memory, despite its apparent complexities, will eventually prove to be simple: a single molecule. He may be right. Small has already discovered a molecule in the dentate gyrus that accounts for cognitive aging. “It regulates how a cell produces new proteins. When the molecule is down [i.e., malfunctions], there are memory problems.”
Separately, while examining the entorhinal cortex cell by cell, Small happened upon the gene sorLA. It had recently been discovered by the geneticist Richard Mayeux, and appeared to be a primary factor causing the risk of late-onset Alzheimer’s disease. The gene is part of something called the retromer complex, a kind of transport system in the entorhinal cortex. When the retromer complex malfunctions, you have what Small describes as “a backlog of cargo,” and excessive amounts of beta-amyloid build up in the brain. This finding was a major breakthrough, one in which discrete pieces of the Alzheimer’s puzzle converged. Small’s observation of how sorLA operates in the retromer complex may eventually lead to the development of an effective treatment for Alzheimer’s, though not in the immediate future. The side effects in the rest of the body when levels of sorLA are manipulated are still unknown.
The “good news” of Halpern’s subtitle is not a stab at false optimism. During the years that she was writing this book, one incontrovertible means of neurogenesis came to light: aerobic exercise. The mechanics of the process couldn’t be simpler: exercise promotes new cell growth in old brains by increasing their blood volume, and cell growth improves memory. It was true for mice with cognitive impairment and it was true for humans with MCI. It didn’t take away amyloid plaque, but it improved cognition anyway. “In addition,” explains Halpern,
exercise…increased the amount of the chemical BDNF (brain-derived neurotrophic factor) circulating in the brain, and it was BDNF that stimulated the birth of new brain cells…. BDNF also enhanced neural plasticity, which was to say that it enabled the brain to prosper. In diseases like Alzheimer’s, depression, Parkinson’s, and dementia more generally, BDNF levels were low. In people who exercised, BDNF levels rose.
There is heartening news, too, for people worried about normal forgetfulness. The Johns Hopkins white paper on memory tells us that “older people who do poorly on timed tests actually do as well or better than their college-age counterparts when they are permitted to work at their own pace.” This is because as we age we recruit the left side of the prefrontal cortex into action, whereas when we are younger we rely mainly on the right side, a phenomenon that has been repeatedly observed on PET scans and MRIs. The neuropsychologist Elkhonon Goldberg believes that this “bilateralism” is a “physical manifestation of wisdom.” Here is Halpern’s typically conversational summary of Goldberg’s argument:
The right side of the brain is where we encounter new and novel situations—it is where we struggle to understand; it is the hemisphere of youth and inexperience. But then we get it. The light goes on. That’s the left side, making the connections, the left side, where the patterns of experience eventually come to reside. Pattern recognition, a left-hemisphere attribute, allows us to chance upon the world with a measure of omniscience—call it wisdom—because what we are encountering is already in us.
An illustration, perhaps, of what Yeats was referring to when he lamented, on turning fifty, the disappearance of the mysterious “dark leopards of the moon,” and the ascendance of “the timid sun.”
Can’t Remember What I Forgot is a virtuosic work of journalistic synthesis. In spite of the certainties and empirical trappings of scientific research, Halpern reminds us that it is a collection of stories like any other, each following its own plot line. Her accomplishment is to have drawn out the myriad threads of these stories, connecting them when possible, to produce a panoramic portrait of an intricate and largely unknown world. Some 106 million people worldwide will be afflicted with Alzheimer’s disease by 2050, 16 million of them Americans, a health crisis that is the result of a triumph of medical science: longer life expectancy in developed countries. Halpern is attuned to the paradox of treating memory, a basic aspect of the self, as a biological puzzle. But she also knows that if the agony of severe memory loss is ever to be relieved, it will be by scientists trawling the brain one molecule at a time.
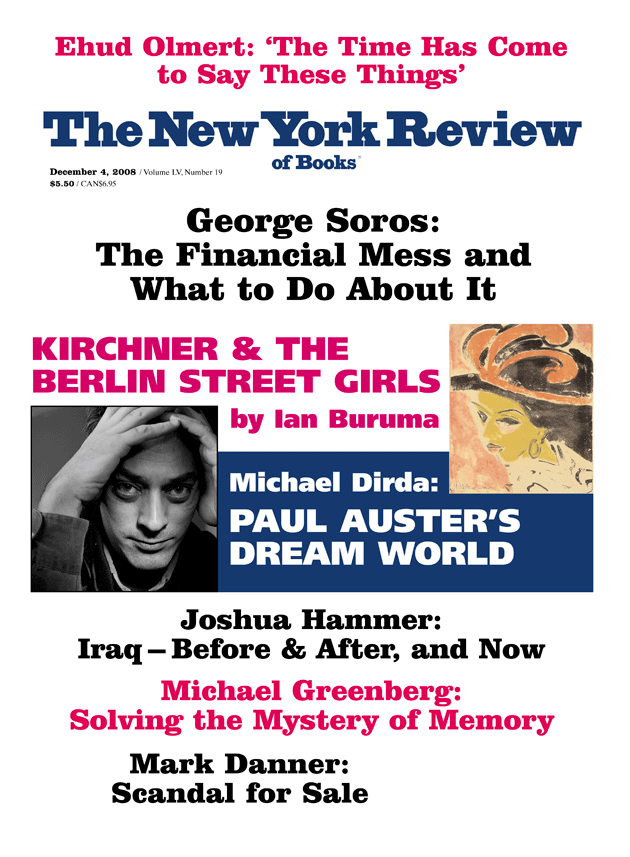
This Issue
December 4, 2008
The Crisis & What to Do About It
‘The Time Has Come to Say These Things’
-
1
Hagar Gelbard-Sagiv, Roy Mukamel, Michal Harel, Rafael Malach, Itzhak Fried, “Internally Generated Reactivation of Single Neurons in Human Hippocampus During Free Recall,” Science, October 3, 2008, pp. 96–101. ↩
-
2
According to a National Institute of Mental Health study cited by Halpern, starting at age sixty-five the average American’s chance of developing Alzheimer’s disease is 10 percent. About half the people who reach age eighty-five experience “diagnosable symptoms.” In public discussions about Alzheimer’s it is often said that 5 percent of Americans already have the disease, though some may still be asymptomatic. If true, this is almost twice as many as suffer from manic-depressive psychosis and schizophrenia combined. ↩
-
3
Nancy L. Mace and Peter V. Rabins, The 36-Hour Day: A Family Guide to Caring for People with Alzheimer’s Disease, Other Dementias, and Memory Loss in Later Life (Johns Hopkins University Press, fourth edition, 2006), pp. 23, 32, 158. ↩
-
4
See Sue Halpern, “Thanks for the Memory,” The New York Review, October 5, 2006. ↩