This is the book which for some length of time I have been awaiting. Not without trepidation, having lived through those lamentable years that made up what the author calls “the rise and decline of psychosurgery.” Professor Valenstein deals particularly with the mutilating brain operation known as a leucotomy—or, in the US, lobotomy—which was performed on tens of thousands of people before its decline in popularity during the 1950s. Most of the principals who developed this procedure were known to me and although I was little more than a disapproving onlooker, I was never an active protestor, I regret to say.
As Professor Valenstein points out in his scholarly account, the operation of leucotomy did not appear upon the psychiatric scene unheralded. The failure of conservative measures to alleviate the symptoms and behavior of a large and captive population of psychotics encouraged the introduction of procedures some of which were reckless, drastic, traumatic, and crude. As in frustration one kicks or thumps into action a faulty radio, the alienist resorted to measures that in every sense of the word were shocking. During the first thirty years of this century dangerous methods inducing states of hypoglycemia, smothering, suffocation, hypothermia, electroshock, or convulsant drug-intoxication were deliberately employed in cases where mental illness was intractable, distressing, or socially unacceptable. The author quotes the apt remarks of my friend the late Dr. Maurice Partridge.
Bizarre illnesses may require bizarre treatment, and in psychiatry they often get it. They show so often a stubbornness and resistiveness to treatment, they expose so clearly the ignorance of their pathology and aetiology that they arouse aggressive reactions in the baffled and frustrated therapist.
Disapproving of long-winded metaphysical attempts to solve the intrapsychic conflicts of the insane as practiced by analysts, those who were in charge of psychotic patients resorted either to desperate and ill-considered steps or else to studied inactivity.
Those of us whose professional lives had been devoted to helping vicitms of structural disease of the brain were horrified by these somatic treatments, which seemed to create the very problems we were trying to cure. A grim homeopathy, indeed. But, strange to say and reluctant to admit, occasionally such violent interventions seemed to work; or, at any rate, distressing symptoms lessened or even disappeared. No obvious explanation was available or even sought. Res ipsa loquitor, as lawyers say.
Neurological sensitivities had in fact already been blunted by the apparent success during the 1920s of treating cases of general paresis by a malaria-induced fever. Such patients had traditionally come within the province of neurologists and not that of psychiatrists or alienists. A few neurologists, like the distinguished Foster Kennedy, even welcomed the advent of insulin coma in schizophrenia as an offset to Freudian analysis. In his preface to the American edition of Sakel’s monograph on insulin shock therapy, he had written, in 1938, that the scholarship of his time was being “blown away by a new wind” and that “we shall not again be content to minister to a mind diseased merely by philosophy and words.”
All this, and much besides, Professor Valenstein tells us in his recital of the tangled story of the physical approaches to mental illness. It was in such a climate of uncritical complacency that Egas Moniz of Portugal introduced in 1935 a surgical attack upon the psychoses by way of a deliberate destruction of the white matter of the frontal lobes of the brain.
Who was this innovator Egas Moniz? And how did it happen that he, a respected neurologist, allowed himself to become involved in the care of the chronically in sane? The author’s answers to these questions are interesting. Since 1911, Egas Moniz had occupied the chair of neurology at the University of Lisbon. Highly unconventional, well-born, versatile, a thwarted politician, he received his medical training at Coimbra University, with postgraduate study in Paris at the feet of such prominent neurologists as Pierre Marie, Jules Dejerine, Josef Babinski, and, particularly, Jean Sicard. Already he had attained fame through his invention of cerebral arteriography, which demonstrated graphically the pattern of the arteries of the brain—a valuable diagnostic aid. This discovery led to flattery from Babinski, who proclaimed that Moniz had set forth on the enterprise as courageously as his compatriots of the fifteenth century, the explorers Bartholomeu Diaz and Vasco da Gama. He was being extravagant in his praise, for to design a clinical device entails ingenuity rather than inspiration.
From the evidence available, it seems likely that the stimulus to his venture into a surgical treatment of the insane was the Second International Congress of Neurology held in London in the summer of 1935. One entire day’s deliberation was devoted to the topic of the frontal lobes of the human brain. The contributions set off in his mind ideas that he debated with his young colleague, Pedro Almeida Lima. They had been hearing at the congress—as I well recall—how surgical “ablation,” or removal, of the frontal lobe in tumor patients was sometimes followed by an unempected change for the better in their mental symptoms. Could it be that deliberate destruction might, therefore, prove an effective remedy for psychotics whose behavior was uninhibited and unmanageable? Such dangerous thinking was unusual for a neurological physician whose responsibility did not ordinarily entail the care of schizophrenics and “cyclothymes,” i.e., people suffering from manic-depressive psychosis.
Advertisement
Back home in Lisbon, Moniz could not rid his mind of these notions and sought an opportunity for putting them to the test. Without delay he secured the transfer to his service of a few mentally deranged patients from the local lunatic asylum. Within a couple of months he was able to publish in several medical journals the results of the destruction of the frontal lobes in twenty patients. In the first seven, he instilled absolute alcohol into the substance of the brain, but afterward he rejected this procedure in favor of a blind sectioning of the white matter with a narrow knife or “leucotome” introduced by way of six trephine holes bored into the most forward part of the skull. This intervention he called a “leucotomy,” the first step in “psychosurgery,” as Moniz put it.
Not only was Moniz no psychiatrist, he was no surgeon. Because of chronic gout his hands were crippled and deformed; he therefore instructed his colleague, Almeida Lima, to act as a technician working under his direction.
Moniz claimed he had been pondering over psychosurgery for several years previously, though there is no written evidence to support this contention, either from him or from any of his colleagues in Portugal. Valenstein is critical of Moniz—and rightly so—on several counts: the haste with which he embarked upon these drastic measures; the lack of careful case selection; an inadequacy in documentation; and the paucity of follow-up studies. Certainly publication was far too precipitous. We may also add the element of imprudence, a trait which sometimes masquerades as courage or boldness.
The author stresses that the hypothesis behind psychosurgery was based upon the flimsiest of reasoning. On the assumption that thoughts and ideas are somehow stored in the frontal lobes among the fibers that connect nerve cells, serious mental disorders were attributed to “fixed thoughts” that had become established to an abnormal degree, and could not be dealt with except by their destruction.
In the interesting biographical account of Egas Moniz written by Antonio Damasio, one-time neurologist in Lisbon, we learn rather more about the personality of Moniz.* He was a lifelong gambler, something that implies an innate recklessness. As to his views on frontal lobe function, Damasio wrote:
Moniz was the organicist par excellence and he clearly conceived psychiatry as a kind of desert soon to be invaded by neurology. Although his approach was sometimes crudely mechanistic, it was not unlike that of a present day cybernetician. He thought, for instance, that ideas were linked to a certain circuit or set of circuits which tended to become fixed by conditioning.
Thus Moniz rationalized his experimental surgery. With the minimum of preparation, with no animal studies to test the safety or otherwise of the procedure, Moniz went on further to justify his undertaking. His admirers generally claimed that creative genius enabled him to see beyond all the possible risks and opposing arguments. Valenstein asserts that there was nothing about any of his arguments that should have persuaded a prudent man to attempt psychosurgery. “It was not genius that enabled Moniz to see beyond the risks; rather, it was his willingness to take these risks.”
Of the twenty patients who were leucotomized, he claimed that seven “recovered,” seven “improved,” while six were “unchanged.” Four of the twenty patients had been referred to him by his friend Sobral Cid, the professor of psychiatry at the University of Lisbon. Dr. Cid, however, soon betrayed a disapproval of his colleague’s venture, and thereafter refused to cooperate. Neither did Moniz secure the backing of the other outstanding neurologists in Lisbon—Dr. António Flores and Dr. Diogo Furtado. After an initial period of cooperation, serious hostility developed between the latter and Professor Moniz.
The patients who were said to have improved were those suffering not from mental derangement but from anxiety and depression. Chronic schizophrenics with marked thought disorders benefited little, if at all. The statement that seven of the patients were “cured” does not convince Valenstein, who considers the accounts that were made available of their postoperative state as being wholly inadequate. The most glaring deficiency, in his opinion, was the brevity of the follow-up period.
Moniz claimed that his operation neither interfered with intelligence nor impaired memory, without, however, giving any data in support. In June 1936 when his monograph was published in Paris it was nonetheless acclaimed widely. Thereafter the operation of leucotomy was practiced on a considerable scale.
Advertisement
From Professor Valenstein’s book we cannot determine how long Moniz and Lima continued to perform leucotomies in Portugal. Moniz retired from his university post in 1944 when he reached the age of seventy, and his chair devolved upon the gifted and scholarly António Flores, who was “critical of Moniz’s venture into the unknown” (Damasio). Moniz continued to write until his death in 1955.
Psychiatrists and neurosurgeons in other parts of the world were not slow to adopt the procedures of leucotomy. Cases were reported in Brazil, Cuba, Romania, and Great Britain, but the majority of operations took place in Italy. Various modifications in technique came about, according to the whims of the surgeons involved.
In pursuance of this grisly saga, we find the center of activity moving from Lisbon to Washington, DC, where, in 1936, the neurologist Walter Freeman read with excitement the accounts of what Moniz had been doing. Although not a surgeon, he determined to adopt the technique immediately after his return from vacation. Perhaps it would not be inappropriate to speak of him as jumping on the bandwagon. He enlisted the interest of his neighbor James Watts, a neurosurgeon, while ordering from a Paris firm of instrument makers two “leucotomes” as devised by Moniz. He also sent Moniz a congratulatory letter, to which came a friendly reply as well as a signed copy of the monograph on leucotomy.
Freeman and Watts jointly operated upon a selected patient in the fall of 1936, and were so pleased with the result that they published an account of the event immediately. Five more patients were then operated upon, and Freeman and Watts presented their results before medical audiences in Baltimore and Chicago. Their reception was a mixed one, especially in Chicago, but Freeman and Watts continued to operate and to lecture on the subject throughout the United States. By the end of 1936 they had operated on twenty people, and they completed another twelve operations in 1937. Technical complications and mishaps occurred at times; for example, snapping of the blade of the leucotome, serious bleeding, and postoperative epilepsy. It therefore became necessary to make some minor changes in their surgical technique, including the placement of the trephine openings and the direction of the intracerebral cuts.
It is perhaps characteristic of a pioneer who is not also the actual instigator of a new idea to alter the accepted terminology. So Freeman proceeded to change what the Europeans had been calling “leucotomy” in favor of “lobotomy,” a term which was accepted in North America but not elsewhere. Great interest was aroused throughout the United States, and psychosurgery was employed even in internationally famed medical centers. There were several reasons for this great popularity:
(a) In many cases an unexpected, even dramatic, change for the better came about in patients with chronic psychoses, hospitalized for years, who had resisted not only conservative lines of treatment but also courses of insulin coma as well as electroshock. To speak of “cure” would not be appropriate. But often a docile state of passivity would replace active symptoms of aggression, anxiety, hypomania, antisocial conduct, obsessional ideas or behavior. In other words, such patients were rendered more easily nursed, and quite often it became possible for them to be discharged home after years of incarceration within a mental asylum.
(b) There was, in such cases, an easing of the financial burden imposed upon the families of the patient, or, in the case of long-staying institutionalized sufferers, the taxpayers.
(c) The operation itself was rapidly performed, being relatively simple, entailing little surgical skill. The mortality was low.
(d) Psychiatrists had in the past been either inactive in the face of these long-staying patients with severe problems, or they had not been successful with their nonsurgical somatic therapy.
(e) Psychosurgery commended itself to the psychiatrists and others who were hostile toward (or disillusioned with) Freudian theories of causation and treatment.
(f) Psychosurgery was also welcomed with varying degrees of warmth by those who held that most forms of insanity were the product of organic, that is, structural, brain pathology of an obscure nature.
(g) Psychosurgery as a news item was a boon to the press. The publicity attendant upon the employment of lobotomy for the considerable population of the mentally deranged was enormous, and there seems to be no evidence that Freeman was embarrassed on this account or that he took any active steps to restrain it.
These considerations prevailed in the 1930s, in spite of the doubts and demurrals of an ethical kind entertained by theologians of various persuasions, humanists, social philosophers, and certain religious and political minority groups. Grave concern was voiced whether submission to “treatment” with psychosurgery could be made compulsory in cases of criminal psychopaths and recidivists. Professor Valenstein sets out these serious arguments, but does not go into the detail that one would have welcomed.
In the debates on psychosurgery Freeman was the devil’s advocate—some would prefer the term “crusader”—dominating his diffident colleague Watts. Lobotomy became a popular, even spectacular, event throughout Europe and the Americas. The first lobotomy in the United States took place on September 14, 1936. Between that date and August 15, 1949, there had been 10,706 lobotomies in the US, according to a survey by C.C. Limburg which is cited by Valenstein.
Freeman, in January 1949, arranged a postgraduate course in psychosurgery, held at the George Washington University School of Medicine. The previous year he had enthusiastically organized the First International Conference on Psychosurgery in Lisbon, with the now aged Egas Moniz presiding. Mutual gestures of acclaim took place. Moniz invested Freeman with the gold chain and medal of the Lisbon Academy of Science, while in the wings steps were being initiated to recommend Moniz for a Nobel Prize. He received the award fourteen months later.
This chronicle of shame reached its lowermost depths in January 1946, when Freeman put into practice a horrendous modified lobotomy that Fiamberti, a psychiatrist in Italy, had been employing since 1937. The new operation was “transorbital lobotomy.” The technique consisted in the introduction of a trocar (or stout hollow needle) above the patient’s eyeball and the optic nerve, piercing the bony roof of the orbit and so gaining access to the white matter of the frontal lobe. Fiamberti would then proceed to destroy the brain tissue by injecting some corrosive fluid such as absolute alcohol or formalin. Freeman preferred to thrust and cut, and made use not of a trocar but of an ordinary ice pick.
Professor Valenstein reproduces a letter from Freeman to his son, which in its graceless tone is illuminating.
I have also been trying out a sort of half-way stage between electroshock and prefrontal lobotomy…. This consists of [sic] knocking them out with a shock and while they are under the “anesthetic” thrusting an ice pick up between the eyeball and the eyelid through the roof of the orbit actually into the frontal lobe of the brain and making the lateral cut by swinging the thing from side to side. I have done two patients on both sides and another on one side without running into any complications, except a very black eye in one case. There may be trouble later on but it seemed fairly easy, although definitely a disagreeable thing to watch. It remains to be seen how these cases hold up, but so far they have shown considerable relief of their symptoms, and only some of the minor behavior difficulties that follow lobotomy. They can even get up and go home within an hour or so. If this works out it will be a great advance for people who are too bad for shock but not bad enough for surgery.
From this letter it is obvious that Freeman must have had in his office or consulting room an apparatus for administering electroshock treatment. This is astounding, for it means that Freeman, ostensibly a “pure” neurologist, must for some time have been accepting and treating psychotic patients over and above those he lobotomized.
This new operation was soon carried out widely throughout the US though not in the old world. Even in Italy it had dwindled. Freeman was of the opinion that the technique of transorbital lobotomy had the advantage of being within the competency of any psychiatrist without surgical skills. The cooperation of neurosurgeons could be bypassed, unless, of course, there were complications. Moreover, hospital attendance was not necessary and the lobotomy could be—and was—carried out in a patient’s home or in the doctor’s office. All this was repugnant to his colleague Watt, and resulted in the breakup of their long personal association.
The press seized upon this novel and startling form of “treatment” and eagerly gave it publicity. This went unchecked by Freeman. He toured the country, visiting mental hospitals, demonstrating his skill on selected patients and teaching the medical staff how to carry out lobotomies themselves. Untoward complications were, it seems, few in number, but occasions there certainly had been when the patient had to be rushed to the hospital because of bleeding, or even because the ice pick had broken within either the orbit or the cavity of the skull. It became necessary to replace the ice pick with a stouter instrument and to employ an ordinary carpenter’s hammer to drive the point of the instrument through the tough bone separating the orbit from the interior of the cranium. We are not told whether actual damage to the eyeball itself ever happened.
Walter Freeman lived until 1972, but in the mid-1950s and after there was a sudden decrease in the number of lobotomies, transorbital and prefrontal, carried out in America and elsewhere. This form of treatment today is but an episode in medical history.
What happened? Events mirror the disappearance of malaria thereapy in general paresis after Alexander Fleming and his co-workers discovered penicillin and its properties. In 1950 French pharmaceutical chemists perfected chlorpromazine, which Delay and Deniker discovered was of benefit to certain psychotic patients, with results comparable to the most successful of the lobotomies. The new remedy was slower in action but it proved to be more consistent that surgery and, of course, nontraumatic. No longer was it deemed necessary to sacrifice brain tissue, and run the risk of lifelong posttraumatic mental syndromes, as well as epilepsy. Chemists were stimulated to explore this promising field, and over the next thirty years there emerged a diversity of psychotropic drugs. Though not wholly devoid of side effects, these drugs are likely to endure; the present formulas will no doubt be followed by other preparations more flexible and more efficient.
The foregoing narrative describes the rise and decline of psychosurgery as surveyed by the author. In my opinion, Professor Valenstein has produced a serious historical document, deeply researched and well-written. It is disturbing without being sensational. The work seemingly is an expansion of a lecture delivered at the University of Cambridge. Why, we ask, did he select this particular topic as the theme of his address? Was it meant to be a simple narration of a disagreeable chapter in medical therapeutics? Was it intended to be on a par with other such dark episodes as the witch-craft trials in New England, the Black Death, or the dancing mania? The author explains that it is a cautionary tale. Is it written in sorrow or in anger? Do we detect an undercurrent of reproach directed toward the discipline of medicine generally? I hope not.
In the first chapter, the author offers us, as a possible explanation of the climate of opinion that made lobotomy possible, his own ideas about the relationship between neurology, neurosurgery, psychiatry, and psychoanalysis. In his opinion, “for lack of a unique therapeutic method, the domain of neurology was shrinking.” He quotes Valenstein on Harvey Cushing, who believed that “neurology was being squeezed by psychiatry on one side and neurosurgery on the other.” Professor Valenstein goes on to say:
This development had clear economic consequences…. Neurologists were finding it difficult to earn a living practicing clinical neurology alone. Some neurologists obtained training in psychiatry and neurological surgery in order to survive.
Were this literally so—which I doubt—it certainly did not apply to countries outside the US. Nor does it tally with the present state of affairs. Neurologists have always been few in number, while far more psychiatrists are required in order to satisfy the needs of the community. Within the domain of medicine, neurology has always occupied a privileged position of elitism; neurosurgeons and psychiatrists came later and have not yet allied themselves as closely with the philosophy of science.
It has happened at times that some clinical neurologists have strayed into the territory of psychiatry, Sigmund Freud being the obvious example. Egas Moniz and Walter Freeman are two others and they illustrate the dangers that attend such forays. In other words, the origins of psychosurgery stem from the meddle-some incursion by a few neurologists into disciplines that were not theirs to invade.
When in 1936 news of the novel operation of leucotomy reached America, doubts were expressed by many senior neurologists and others. Some, however, were less than forthright in their condemnation. Thus Adolf Meyer, the Nestor among psychiatrists in the United States, declared,
I am not antagonistic to this work but find it very interesting. I have some of those hesitations about it that are mentioned by other discussants, but I am inclined to think that there are more possibilities in this operation than appear on the surface.
These cautious remarks coming from one of his authority were taken as an encourgement, as Professor Valenstein has indicated. Stanley Cobb the respected Boston neuropsychiatrist pronounced darkly: “In my opinion this is a justifiable procedure only when the patient is old and the prognosis hopeless. Specifically, I can recommend the operation only in cases of prolonged agitated depression in persons over 60 years of age.” In other words, the results being permanent, the shorter the better. An odd moral judgment indeed.
Some readers may consider that Professor Valenstein has gone too far in his condemnation of psychosurgery. They may protest that the award of a Nobel Prize to the inventor surely testifies to the magnitude of his contribution to medicine. I do not agree. Homer has been known to nod, and this most prestigious award has, in retrospect, not always been bestowed wisely.
In the final chapter of this book, Professor Valenstein deals critically with the contemporary surgical treatment of patients with heart disease. This I cannot support, for a judgment upon matters cardiological is far outside my province, and, I suspect, that of the author as well. But in the great majority of the author’s opinions, disturbing though they are, I sadly concur. He holds the view that the factors that fostered the development of psychosurgery are active today, being “part of the very bone and marrow of the practice not only of psychiatry but of all medicine.” He stresses the harm that has been caused by premature claims of cures, by unbridled ambition, and by uncritical enthusiastic promotion.
Harsh words indeed, but not to be brushed aside. Today, when medicine aspires to become a science, it behooves those of us who are clinicians never for a moment to lose sight of the fundamental duty of our art and mystery—primum non nocere. Never let us forget the plea of that wisest of physicians, Sir Robert Hutchison.
From the inability to let well alone; from too much zeal for the new and contempt for what is old; from putting knowledge before wisdom, science before art, and cleverness before commonsense; from treating patients as cases, and from making the cure of the disease more grievous than its endurance, good Lord, deliver us.
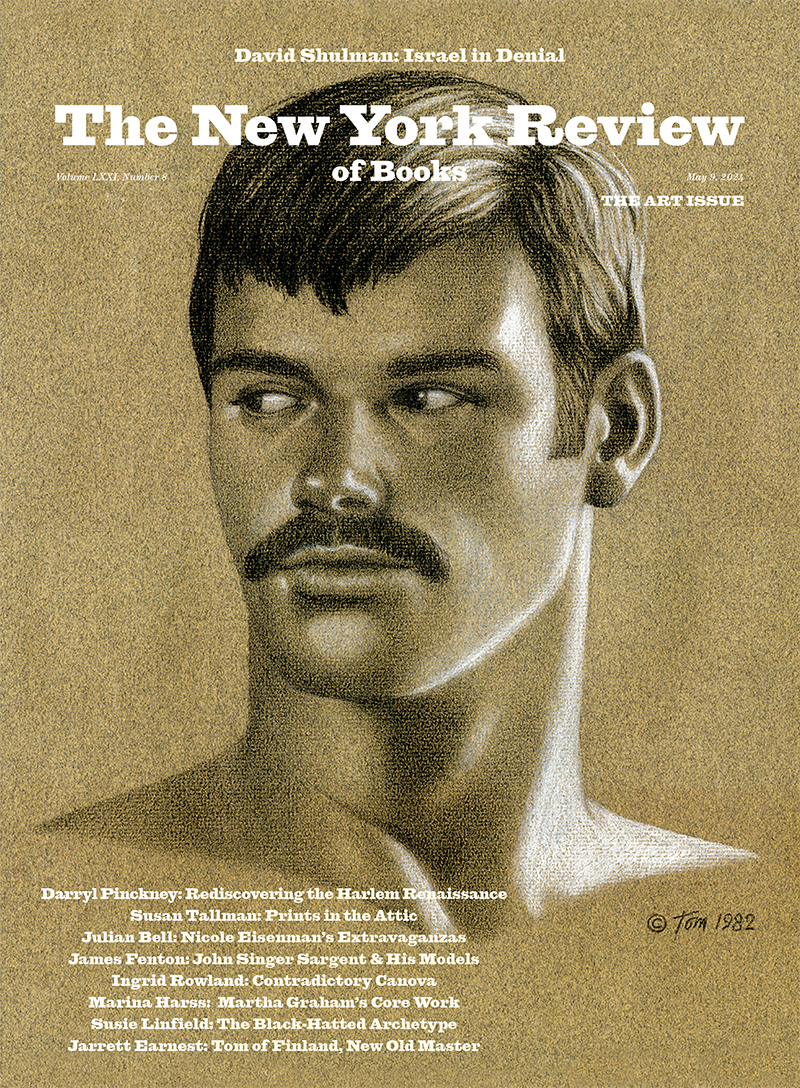
This Issue
April 24, 1986
-
*
“Egas Moniz, Pioneer of Angiography and Leucotomy,” Mt. Sinai Journal of Medicine (1975), pp. 500–513. ↩