Over the past fifteen years, transplanting human organs has become a standard and remarkably successful medical procedure, giving new life to thousands of people with failing hearts, kidneys, livers, and lungs. But very few countries have sufficient organs to meet patients’ needs. In the United States, for example, some 50,000 people are on the waiting list for a transplant; fifteen percent of patients who need a new heart will die before one becomes available. The shortages are even more acute throughout the Middle East and Asia.
This lack of available organs arouses desperation and rewards greed. Would-be recipients are willing to travel far to get an organ and many surgeons, brokers, and government officials will do nearly anything to profit from the shortage. In India well-to-do people and their doctors buy kidneys from debt-ridden Indian villagers; in China officials profitably market organs of executed Chinese prisoners. The international commerce in organs is unregulated, indeed anarchic. We know a good deal about trafficking in women and children for sex. We are just beginning to learn about the trafficking in organs for transplantation.
1.
The routes that would-be organ recipients follow are well known to both doctors and patients. Italians (who have the lowest rate of organ donation in Europe) travel to Belgium to obtain their transplants; so do Israelis, who lately have also been going to rural Turkey and bringing their surgeon along with them. Residents of the Gulf States, Egyptians, Malaysians, and Bangladeshis mainly go to India for organs. In the Pacific, Koreans, Japanese, and Taiwanese, along with the residents of Hong Kong and Singapore, fly to China. Less frequently, South Americans go to Cuba and citizens of the former Soviet Union go to Russia. Americans for the most part stay home, but well-to-do foreigners come to the United States for transplants, and some centers allot up to 10 percent of their organs to them.
All of these people are responding to the shortages of organs that followed on the discovery of cyclosporine in the early 1980s. Until then, transplantation had been a risky and experimental procedure, typically a last-ditch effort to stave off death; the problem was not the complexity of the surgery but the body’s immune system, which attacked and rejected the new organ as though it were a foreign object. Cyclosporine moderated the response while not suppressing the immune system’s reactions to truly infectious agents. As a result, in countries with sophisticated medical programs, kidney and heart transplantation became widely used and highly successful procedures. Over 70 percent of heart transplant recipients were living four years later. Ninety-two percent of patients who received a kidney from a living donor were using that kidney one year later; 81 percent of the cases were doing so four years later, and in 40 to 50 percent of the cases, ten years later.1
Transplantation spread quickly from developed to less developed countries. By 1990, kidneys were being transplanted in nine Middle Eastern, six South American, two North African, and two sub-Saharan African countries. Kidney transplants are by far the most common, since kidney donors can live normal lives with one kidney, while kidneys are subject to disease from a variety of causes, including persistent high blood pressure, adult diabetes, nephritis (inflammation of vessels that filter blood), and infections, which are more usually found in poor countries. (It is true that the donor runs the risk that his remaining kid-ney will become diseased, but in developed countries, at least, this risk is small.) The transplant techniques, moreover, are relatively simple. Replacing one heart with another, for example, is made easier by the fact that the blood-carrying vessels that must be detached from the one organ and reattached to the other are large and relatively easy to handle. (A transplant surgeon told me that if you can tie your shoes, you can transplant a heart.)
Fellowships in American surgical programs have enabled surgeons from throughout the world to master the techniques and bring them home. Countries such as India and Brazil built transplant centers when they might have been better advised to invest their medical resources in public health and primary care. For them the centers are a means for enhancing national prestige, for persuading their surgeons not to leave the country, and for meeting the needs of their own middle-class citizens.
In China, more than fifty medical centers report they perform kidney transplants, and in India hundreds of clinics are doing so. Reliable information on the success of these operations is hard to obtain, and there are reports that hepatitis and even AIDS have followed transplant operations. But according to physicians I have talked to whose patients have traveled to India or China for a transplant, and from published reports within these countries, some 70 to 75 percent of the transplants seem to have been successful.2
With patient demand for transplantation so strong and the medical capacity to satisfy it so widespread, shortages of organs were bound to occur. Most of the doctors and others involved in early transplants expected that organs would be readily donated as a gift of life from the dead, an exchange that cost the donor nothing and brought the recipient obvious benefits. However, it turns out that powerful cultural and religious taboos discourage donation, not only in countries with strong religious establishments but in more secular ones as well. The issue has recently attracted the attention of anthropologists, theologians, and literary scholars, and some of their findings are brought together in the fascinating collection of essays, Organ Transplantation: Meanings and Realities.3
Advertisement
In the Middle East, it is rare to obtain organs from cadavers. Islamic teachings emphasize the need to maintain the integrity of the body after death, and although some prominent religious leaders make an exception for transplants, others refuse. An intense debate occurred last spring in Egypt when the government-appointed leader of the most important Sunni Muslim theological faculty endorsed transplantation as an act of altruism, saying that permitting it was to accept a small harm in order to avoid a greater harm—the same rationale that allows a Muslim to eat pork if he risks starvation. But other clerics immediately objected, and there is no agreement in favor of donation.
In Israel, Orthodox Jewish precepts define death exclusively as the failure of the heart to function, not the cessation of brain activity, a standard that makes it almost impossible to retrieve organs. The primary purpose of statutes defining death as the absence of brain activity is to ensure that organs to be transplanted are continuously supplied with oxygen and nutrients; in effect, the patient is declared dead, and a respirator keeps the heart pumping and the circulatory system working until the organs have been removed, whereupon the respirator is disconnected. Some rabbis give precedence to saving a life and would therefore accept the standard of brain death for transplantation. But overall rates of donation in Israel are very low. The major exceptions are kibbutz members, who tend to be community-minded, as well as other secular Jews.
In much of Asia, cultural antipathy to the idea of brain death and, even more important, conceptions of the respect due elders, have practically eliminated organ transplantation. For all its interest in new technology and its traditions of gift-giving, Japan has only a minuscule program, devoted almost exclusively to transplanting kidneys from living related donors. As the anthropologist Margaret Lock writes: “The idea of having a deceased relative whose body is not complete prior to burial or cremation is associated with misfortune, because in this situation suffering in the other world never terminates.”4 For tradition-minded Japanese, moreover, death does not take place at a specific moment. The process of dying involves not only the heart and brain but the soul, and it is not complete until services have been held on the seventh and forty-ninth days after bodily death. It takes even longer to convert a deceased relative into an ancestor, all of which makes violating the integrity of the body for the sake of transplantation unacceptable.
Americans say they favor transplantation but turn out to be very reluctant to donate organs. Despite countless public education campaigns, organ donation checkoffs on drivers’ licenses, and laws requiring health professionals to ask families to donate the organs of a deceased relative, the rates of donation have not risen during the past five years and are wholly inadequate to the need. As of May 1997, according to the United Network for Organ Sharing, 36,000 people were awaiting a kidney transplant, 8,000 a liver transplant, and 3,800 a heart transplant.5 One recent study found that when families were asked by hospitals for permission to take an organ from a deceased relative, 53 percent flatly refused.
The literary critic Leslie Fiedler suggests that the unwillingness of Americans to donate organs reflects an underlying antipathy to science and a fear of artificially creating life, a fear exploited, he suggests, in the many Hollywood remakes of the Frankenstein story. Moreover, donation would force Americans to concede the finality of death, which Fiedler is convinced they are reluctant to do.6 I suspect, however, that the underlying causes are less psychological than social. Americans are unaccustomed to sharing resources of any kind when it comes to medicine. Since Americans refuse to care for one another in life—as witness the debacle of national health insurance—why would they do so in death? Receiving help is one thing, donating it is another.
2.
If organs are in such short supply, how do some countries manage to fill the needs of foreigners? The answers vary. Belgium has a surplus of organs because it relies upon a “presumed consent” statute that probably would be rejected in every American state. Under its provisions, you must formally register your unwillingness to serve as a donor; otherwise, upon your death, physicians are free to transplant your organs. To object you must go to the town hall, make your preference known, and have your name registered on a national computer roster; when a death occurs, the hospital checks the computer base, and unless your name appears on it, surgeons may use your organs, notwithstanding your family’s objections. Iwas told by health professionals in Belgium that many citizens privately fear that if they should ever need an organ, and another patient simultaneously needs one as well, the surgeons will check the computer and give the organ to the one who did not refuse to be a donor. There is no evidence that surgeons actually do this; still many people feel it is better to be safe than sorry, and so they do not register any objections.
Advertisement
One group of Belgian citizens, Antwerp’s Orthodox Jews, have nonetheless announced they will not serve as donors, only as recipients, since they reject the concept of brain death. An intense, unresolved rabbinic debate has been taking place over the ethics of accepting but not giving organs. Should the Jewish community forswear accepting organs? Should Jews ask to be placed at the bottom of the waiting list? Or should the Jewish community change its position so as to reduce the prospect of fierce hostility or even persecution?
Because its system of presumed consent has worked so well, Belgium has a surplus of organs and will provide them to foreigners. However, it will not export them, say, to Milan or Tel Aviv, which would be entirely feasible. Instead, it requires that patients in need of a transplant come to Belgium, which then benefits from the surgical fees paid to doctors and hospitals.
Not surprisingly, money counts even more in India, which has an abundant supply of kidneys because physicians and brokers bring together the desperately poor with the desperately ill. The sellers include impoverished villagers, slum dwellers, power-loom operators, manual laborers, and daughters-in-law with small dowries. The buyers come from Egypt, Kuwait, Oman, and other Gulf States, and from India’s enormous middle class (which numbers at least 200 million). They readily pay between $2,500 and $4,000 for a kidney (of which the donor, if he is not cheated, will receive between $1,000 and $1,500) and perhaps two times that for the surgery. From the perspective of patients with end-stage renal disease, there is no other choice. For largely cultural reasons, hardly any organs are available from cadavers; dialysis centers are scarce and often a source of infection, and only a few people are able to administer dialysis to themselves at home (as is also the case in the US). Thus it is not surprising that a flourishing transplant business has emerged in such cities as Bangalore, Bombay, and Madras.
The market in organs has its defenders. To refuse the sellers a chance to make the money they need, it is said, would be an unjustifiable form of paternalism. Moreover, the sellers may not be at greater risk living with one kidney, at least according to US research. A University of Minnesota transplant team compared seventy-eight kidney donors with their siblings twenty years or more after the surgery took place, and found no significant differences between them in health; indeed, risk-conscious insurance companies do not raise their rates for kidney donors.7 And why ban the sale of kidneys when the sale of other body parts, including semen, female eggs, hair, and blood, is allowed in many countries? The argument that these are renewable body parts is not persuasive if life without a kidney does not compromise health. Finally, transplant surgeons, nurses, and social workers, as well as transplant retrieval teams and the hospitals, are all paid for their work. Why should only the donor and the donor’s family go without compensation?
But because some body parts have already been turned into commodities does not mean that an increasing trade in kidneys and other organs is desirable. To poor Indians, as Margaret Radin, professor of law at Stanford, observes, “Commodification worries may seem like a luxury. Yet, taking a slightly longer view, commodification threatens the personhood of everyone, not just those who can now afford to concern themselves about it.” Many of the poor Indians who sell their organs clearly feel they have had to submit to a degrading practice in order to get badly needed sums of money. They would rather not have parts of their body cut out, an unpleasant experience at best, and one that is probably more risky in Bombay than in Minnesota. Radin concludes: “Desperation is the social problem that we should be looking at, rather than the market ban….We must rethink the larger social context in which this dilemma is embedded.”8
In 1994, perhaps for reasons of principle or because of public embarrassment—every world medical organization opposes the sale of organs—a number of Indian states, including the regions of Bombay, Madras, and Bangalore, outlawed the practice, which until then had been entirely legal. But the laws have an egregious loophole so that sales continue almost uninterrupted. A detailed and persuasive report in the December 26, 1997, issue of Frontline, one of India’s leading news magazines, explains how the new system works.9 The legislation permits donations from persons unrelated to the recipient if the donations are for reasons of “affection or attachment,” and if they are approved by “authorization committees.” These conditions are easily met. Brokers and buyers coach the “donors” on what to say to the committee—that he is, for example, a cousin and that he has a (staged) photograph of a family gathering to prove it, or that he is a close friend and bears great affection for the potential recipient. Exposing these fictions would be simple enough, but many committees immediately approve them, unwilling to block transactions that bring large sums to hospitals, surgeons, and brokers.
Accurate statistics on kidney transplantation in India are not available, but Frontline estimates that about one third of transplants come from living, unrelated donors; four years after the new law went into effect, the rate of transplantation has returned to its earlier levels. It is true that not every hospital participates in the charade, that the market in kidneys is less visible than it was, and it may well be that fewer foreigners are coming to India for a transplant. But the lower classes and castes in India, already vulnerable to so many other abuses, continue to sell their organs. As Frontline reports, many donors who sell their organs do so because they are badly in debt; and before long they are again in debt.
3.
China is at the center of the Pacific routes to organ transplantation because it has adopted the tactic of harvesting the organs of executed prisoners. In 1984, immediately after cyclo-sporine became available, the government issued a document entitled “Rules Concerning the Utilization of Corpses or Organs from the Corpses of Executed Prisoners.” Kept confidential, the new law provided that organs from executed prisoners could be used for transplants if the prisoner agreed, if the family agreed, or if no one came to claim the body. (Robin Munro of Human Rights Watch/Asia brought the law to light.) That the law lacks an ethical basis according to China’s own values is apparent from its stipulations. “The use of corpses or organs of executed prisoners must be kept strictly secret,” it stated, “and attention must be paid to avoiding negative repercussions.” The cars used to retrieve organs from the execution grounds cannot bear health department insignia; the people involved in obtaining organs are not permitted to wear white uniforms. In my own interviews with Chinese transplant surgeons, none would admit to the practice; when I showed them copies of the law, they shrugged and said it was news to them.
But not to other Asian doctors. Physicians in Japan, Hong Kong, Singapore, and Taiwan, among other countries, serve as travel agents, directing their patients to hospitals in Wuhan, Beijing, and Shanghai. The system is relatively efficient. Foreigners do not have to wait days or weeks for an organ to be made available; executions can be timed to meet market needs and the supply is more than adequate. China keeps the exact number of executions secret but Amnesty International calculates on the basis of executions reported in newspapers that there are at least 4,500 a year, and perhaps three to four times as many. Several years ago a heart transplant surgeon told me that he had just been invited to China to perform a transplant; accustomed to long waiting periods in America, he asked how he could be certain that a heart would be available when he arrived. His would-be hosts told him they would schedule an execution to fit with his travel schedule. He turned down the invitation. In February the FBI arrested two Chinese nationals living in New York for allegedly soliciting payment for organs from executed prisoners to be transplanted in China.
China’s system also has its defenders. Why waste the organs? Why deprive prisoners of the opportunity to do a final act of goodness? But once again, the objections should be obvious. The idea that prisoners on death row—which in China is a miserable hovel in a local jail—can give informed consent to their donations is absurd. Moreover, there is no way of ensuring that the need for organs might not influence courtroom verdicts. A defendant’s guilt may be unclear, but if he has a long criminal record, why not condemn him so that a worthy citizen might live?
To have physicians retrieve human organs at an execution, moreover, subverts the ethical integrity of the medical profession. There are almost no reliable eyewitness accounts of Chinese practices, but until 1994, Taiwan also authorized transplants of organs from executed prisoners, and its procedures are probably duplicated in China. Immediately before the execution, the physician sedates the prisoner and then inserts both a breathing tube in his lungs and a catheter in one of his veins. The prisoner is then executed with a bullet to his head; the physician immediately moves to stem the blood flow, attach a respirator to the breathing tube, and inject drugs into the catheter so as to increase blood pressure and cardiac output. With the organs thus maintained, the body is transported to a hospital where the donor is waiting and the surgery is performed. The physicians have become intimate participants in the executions; instead of protecting life, they are manipulating the consequences of death.
The motive for all such practices is money. The Europeans, Middle Easterners, and Asians who travel to China, India, Belgium, and other countries pay handsomely for their new organs and in hard currencies. Depending on the organization of the particular health care system and the level of corruption, their fees will enrich surgeons or medical centers, or both. Many of the surgeons I interviewed were quite frank about how important the income from transplants was to their hospitals, but they were far more reluctant to say how much of it they kept for themselves. Still, a leading transplant surgeon in Russia is well known for his vast estate and passion for horses. His peers in India and China may be less ostentatious but not necessarily less rich. They will all claim to be doing good, rescuing patients from near death.
4.
The international trade in organs has convinced many of the poor, particularly in South America, that they or their children are at risk of being mutilated and murdered. Stories are often told of foreigners who arrive in a village, survey the scene, kidnap and murder several children, remove their organs for sale abroad, and leave the dissected corpses exposed in the graveyard. In Guatemala in 1993 precisely such fears were responsible for one innocent American woman tourist being jailed for a month, and another being beaten to death.
Villagers’ anxieties are shared by a number of outside observers who believe that people are being murdered for their organs. The author of the report of a transplant committee of the European Parliament unequivocally asserted that
Organized trafficking in organs exists in the same way as trafficking in drugs. It involved killing people to remove organs which can be sold at a profit. To deny the existence of such trafficking is comparable to denying the existence of ovens and gas chambers during the last war.10
So, too, the rapporteur of a UN committee on child welfare circulated a questionnaire asserting that “the sale of children is mainly carried out for the purpose of organ transplantation.” It then asked: “To what extent and in what ways and forms do these violations of children’s rights exist in your country? Please describe.”11
The stories of organ snatching have an American version. I have heard it from my students, read about it on e-mail, been told about it with great conviction by a Moscow surgeon, and been asked about it by more than a dozen journalists. According to the standard account, a young man meets an attractive woman in a neighborhood bar; they have a few drinks, go back to her place, whereupon he passes out and then wakes up the next morning to find a sewn-up wound on his side. When he seeks medical attention, he learns that he is missing a kidney.
Although there have been sporadically reported stories of robberies of kidneys from people in India, I have not found a single documented case of abduction, mutilation, or murder for organs, whether in North or South America. I was in Guatemala in 1993 when the atrocities are alleged to have occurred, and heard seemingly reliable people say there was convincing evidence for them. I stayed long enough to see every claim against the two American women tourists proven false. Nevertheless, as the anthropologist Nancy Scheper-Hughes argues, the villagers’ fears and accusations are understandable in the light of their everyday experience. The bodies of the poor are ordinarily treated so contemptuously that organ snatching does not seem out of character. In Guatemala, babies are regularly kidnapped for sale abroad in the adoption market. Local doctors and health workers admitted to me that “fattening houses” have been set up so that kidnapped babies would be more attractive for adoption.
But it is extremely dangerous to investigate the adoption racket, since highly placed officials in the government and military take a cut of the large sums of money involved. Moreover, Scheper-Hughes continues, if street children in Brazil can be brazenly murdered without recrimination, it is not far-fetched for slum dwellers to believe that the organs of the poor are being removed for sale abroad. And since girls and boys can be kidnapped with impunity to satisfy an international market in sex, why not believe they are also kidnapped to satisfy an international market for organs?12
In truth, medical realities make such kidnappings and murder highly unlikely. The rural villages and the urban apartments in which transplants are alleged to secretly take place do not have the sterile environment necessary to remove or implant an organ. Organs from children are too small to be used in adults. And however rapacious health care workers may seem, highly trained and medically sophisticated teams of surgeons, operating room nurses, anesthesiologists, technicians, and blood transfusers are not likely to conspire to murder for organs or accept them off the street. Had they done so, at least one incident would have come to light during the past fifteen years.
5.
The well-documented abuses are bad enough. Is there some way of diminishing them? The Bellagio Task Force, an international group including transplant surgeons, human rights activists, and social scientists, has made several proposals that might be effective if they could be carried out.13
Almost all major national and international medical bodies have opposed the sale of organs and the transplantation of organs from executed prisoners; but none of the medical organizations has been willing to take action to enforce their views. The World Medical Association in 1984, 1987, and 1994 condemned “the purchase and sale of human organs for transplantation.” But it asks “governments of all countries to take effective steps,” and has adopted no measures of its own. It has also criticized the practice of using organs from executed prisoners without their consent; but it fails to ask whether consent on death row can be meaningful. The association leaves it to national medical societies to “severely discipline the physicians involved.” Neither it nor any other medical organization has imposed sanctions on violators.
The Bellagio Task Force has posed several challenges to the international medical societies. What would happen if they took their proclaimed principles seriously, established a permanent monitoring body, and kept close surveillance on organ donation practices? What if they threatened to withhold training fellowships from countries which tolerated exploitative practices? What if they refused to hold international meetings in those countries, and, as was the case with South Africa under apartheid, did not allow physicians from those countries to attend their meetings? Why, moreover, couldn’t the Novartis company, the manufacturer of cyclosporine, insist that it would sell its product only to doctors and hospitals that meet strict standards in obtaining organs? Such measures would be likely to have a serious effect, certainly in India, probably even in China. But as with the organs themselves, the willingness of doctors to use the moral authority of medicine as a force for change has, so far, been in short supply.
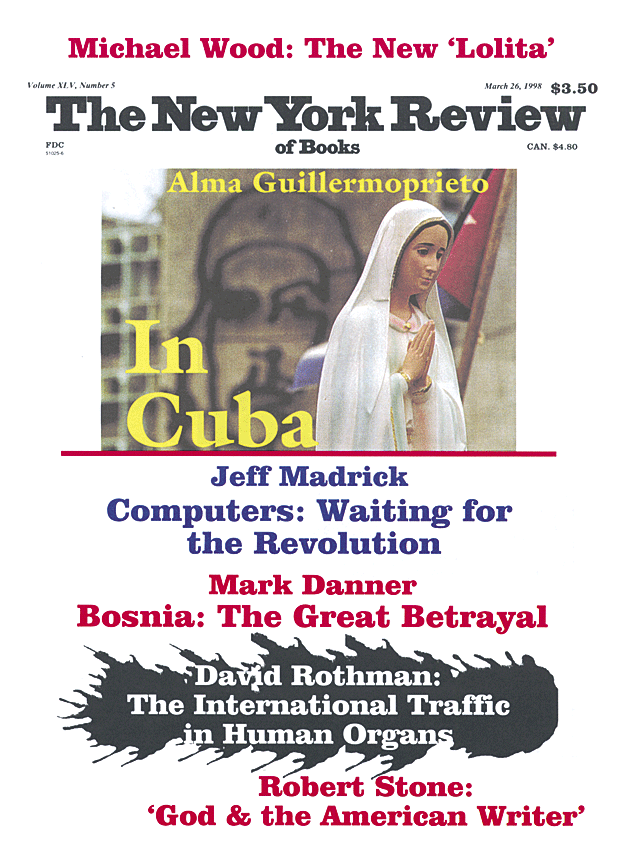
This Issue
March 26, 1998
-
1
The data is from the United Network for Organ Sharing (UNOS) Scientific Registry, as of July 5, 1997. ↩
-
2
Xia Sui-sheng, “Organ Transplantation in China: Retrospect and Prospect,” Chinese Medical Journal, 105 (1992), pp. 430-432. ↩
-
3
Edited by Stuart J. Youngner, Renée C. Fox, and Laurence J. O’Connell (University of Wisconsin Press, 1996). ↩
-
4
“Deadly Disputes: Ideologies and Brain Death in Japan,” in Youngner et al., Organ Transplantation, pp. 142-167. ↩
-
5
According to a recent report on CNN’s Headline News, there are only 4,000 livers a year being donated. In response to the shortage, the UCLA Medical Center has developed a procedure for dividing livers taken from the cadavers of donors, so that two recipients can share it. ↩
-
6
“Why Organ Transplant Programs Do Not Succeed,” in Youngner et al., Organ Transplantation, pp. 56-65. ↩
-
7
John S. Najarian, Blanche M. Chavers, Lois E. McHugh, and Arthur J. Matas, “20 Years or More of Follow-Up of Living Kidney Donors,” Lancet, 340 (October 3, 1992), pp. 807-809. ↩
-
8
Margaret Jane Radin, Contested Commodities (Harvard University Press, 1996), p. 125. ↩
-
9
“Kidneys Still for Sale,” Frontline, 14 (December 13-26, 1997), pp. 64-79. ↩
-
10
This and other examples of lending credence to the rumors may be found in the United States Information Agency Report of December 1994, “The Child Organ Trafficking Rumor,” written by Todd Leventhal. ↩
-
11
Vitit Muntarbhorn, “Sale of Children,” Report of the Special Rapporteur to the United Nations Commission on Human Rights, January 12, 1993. ↩
-
12
Nancy Scheper-Hughes, “Theft of Life: The Globalization of Organ Stealing Rumours,” Anthropology Today, 12 (June 1996), pp. 3-11. ↩
-
13
D.J. Rothman, E. Rose, et al., “The Bellagio Task Force Report on Transplantation, Bodily Integrity, and the International Traffic in Organs,” Transplantation Proceedings, 29 (1997), pp. 2739-2745. I am currently serving as chair of the Bellagio group. ↩