1.
To enter a hospital is to pass into a zone of occasional and unusual danger. Many illnesses invite well-tried treatments with normally uncomplicated outcomes. But unintended catastrophe is always at hand. In John Murray’s unsettling account of life on the intensive care unit at San Francisco General Hospital, one story exemplifies the intrusion of unexpected disaster.
Day 26 of Murray’s month on service. Julius Upshaw, who drinks too much, injects himself with heroin, and earns a lean living as a panhandler, has been admitted three weeks before with an infected human bite. The story is that he has been caught in a brawl, the outcome of which has left his hand trapped between the clenched jaws of his opponent. The human mouth is a paradise for bacteria, and Mr. Upshaw’s swollen hand is now oozing thick pus. Crimson threads—infected lymph vessels—track toward his armpit.
Treatment is straightforward: intravenous antibiotics. But without a ready supply of alcohol, Mr. Upshaw quickly begins to shake uncontrollably from acute withdrawal. He is sedated, and immediately aspirates vomit into his lungs. A nasty pneumonia ensues that, in the presence of a serious blood infection, tips his kidneys into failure. He develops a syndrome in which his entire body swells with fluid, turning him into a ball of human flesh. The retained fluid begins to spill into Mr. Upshaw’s lungs. Quite reasonably, it is decided to remove some of this fluid with a needle to prevent him from drowning. The lung, less reasonably, collapses and surgeons are summoned to place a tube into his now hollow chest cavity. By this time, there is only one safe place for this unlucky patient to go: the intensive care unit.
Murray’s diary of daily patient admissions—sixty in all—puts the reader at the center of the tense decision-making that frequently takes place in a crisis setting. San Francisco General is a tough front-line city hospital for the disadvantaged, founded in 1850 during a bitter cholera epidemic. It faces the raw edge of urban living.
Despite these pressures, Murray’s style is methodical. Each day’s account opens with a brief introduction to a large issue—misdiagnoses, the language of medicine, the threat of infection—which is then illustrated by a case or two from the day’s admissions. Murray ties his narrative together by interweaving the stories of patients already in the ICU with the experiences of his new patients.1 This device enables him to select and discuss aspects of their clinical course that throw light on both the inexact arts of intensive care and intensely personal issues, such as how one dies.
His “chief purpose” is “to inform people about what really goes on in ICUs…. Few have this information, but it concerns everyone.” By writing in depth about this one specialty of medicine, and for a broad general audience rather than for other physicians alone, Murray follows a long twentieth-century tradition of clinical narratives. This genre was inaugurated by William Carlos Williams in The Doctor Stories.2 In essays such as “The Use of Force,” medicine was shown to be a messy affair, with many predicaments that seem far away from the orderly clinic or antiseptic operating room.
The approach that Williams used so well has been further and finely developed by Richard Selzer, a surgeon, who, in books such as Letters to a Young Doctor and Mortal Lessons,3 used the confessional and interpretative essay to describe some of the most unexplored trenches of medicine. An example of a recent new voice in this tradition is Frank Huyler’s The Blood of Strangers.4 This narrative vein of medical writing has become gorged to such a degree that its study has become an academic discipline in its own right.5
But Murray has a larger purpose than simply to develop the heritage of doctor as writer or to open a window for those curious enough to look through. He is disturbed that the view of ICU medicine presented to the public seriously distorts the truth. For instance, the success rate for resuscitations acted out in television series such as ER is 75 percent. The true figure is 15 percent. Murray’s observations—he has worked in intensive care for much of his career—lead him to two conclusions. First, “that death is an ever-present part of the ICU story.” And second, “that death is not a correctable biological condition—it is everyone’s ultimate destiny.”
We might think that ICUs work miracles. They do not. They fail more often than they succeed. That reality is not a comfortable one to admit, but it matters because it forces us to confront issues such as physician-assisted suicide with an honest understanding of what medicine can fairly be expected to achieve. The evidence that Murray accumulates from his sixty patients allows him to construct a persuasive argument. In sum, it is “that the current decision-making process [in ICUs] can and should be improved.”
Advertisement
This critical look at intensive care is a surprising and important departure for Murray. His academic reputation rests largely on his co-editorship of a comprehensive review of respiratory medicine,6 which was first published in 1988. A third edition will come out this year. In the preface to the first edition, Murray and Jay Nadel emphasize their belief in the logical scientific basis of respiratory medicine: “A strong foundation in these basic sciences will make possible a rational and scientific approach to the more specialized clinical material.” In the past twenty years, his research and other writings have concentrated on tuberculosis, HIV, and the interplay between these two lethal infections. In other words, Murray has been a sober academic commentator on a highly technical discipline. Something striking seems to have taken place to lead him to write for a new audience.
Murray’s sardonic description of the tribal nature of hospital life makes his case that much more convincing. He creates a telling picture of the ICU. At the apex of the tribal hierarchy is the attending physician who has overall responsibility for patient care and who gives out “orders” each day. A cadre of young doctors—from confident first-year residents to wiser third-year residents—carry out these instructions, do the scut work, and cover nights while their bosses sleep or, as Murray once admits, sneak off during the day to play the occasional game of tennis. Residents throughout the world have a highly variable sense of respect for their attending physicians. Murray is self-consciously aware that his ways are seen as old-fogeyish by some of his younger colleagues.
Nurses, not doctors, hold the ICU together. They know more about their patients than any doctor and they are frequently more experienced than residents at the technical aspects of ICU care. There are competing specialists too. Surgeons are impatient aggressors, holding their scalpels poised to slice through the procrastinations of dithering colleagues. Murray is sensitive to their highly charged presence:
Surgeons routinely perform technical feats no internist would ever conceive of undertaking, and they bring those brilliant skills with them when they consult on a patient. But they often bring their giant egos and short fuses as well. A surgeon friend of mine has characterized his confreres as “Often wrong, but never in doubt.” By contrast, the call to arms for internists is “Don’t just do something, stand there.” It is undoubtedly good for the profession that it includes men and women of instant action as well as those of prolonged reflection; but when these polar temperaments meet at the bedside of a sick person, things can heat up.
Somehow these tribes do work together, in a balance of often ferocious suspicion.
Doctors also take part in rituals that strengthen their traditional tribal loyalties. At San Francisco General Hospital, as elsewhere, these rituals have included daily ward rounds, morning report, weekly grand rounds with a retinue of residents, and even “liver rounds,” at which a drink or three was taken to celebrate the end of the week. Murray is nostalgic about these rituals because he sees the ethos that they embody—and so the spirit that binds the medical team together—now being irrevocably eroded. Bedside ward rounds are being diminished by the false notion that to discuss a patient’s care next to the patient is somehow demeaning; grand rounds by academic arrogance and the perfidious intrusions of the pharmaceutical industry; and “liver rounds” by the replacement of beer and pretzels with more socially correct ice cream and cookies.
It is in the daily detail of an ICU at work that Murray wonderfully depicts a place of function and dysfunction. His account is based on the stories of his sixty admissions, all with various combinations of failing hearts, lungs, brains, kidneys, livers, and intestines. Causes of death range from bizarre accident (a carrot lodged in a bronchus) to repeated episodes of self-harm (alcohol, heroin, cocaine, and other undiscovered substances) to the familiar ravages of old age (cancer, stroke, and heart attack).
Murray shows that the ICU is a place of small successes rather than triumphant victories. He does not hide the rougher side of intensive care: the need for strong prison-like restraints to tie down agitated patients; the lethal presence of hospital-acquired infections; the crude indignities that a lack of privacy forces on ICU patients and their families; the psychic terrors that afflict some of those under his care; the threats of litigation from worried relatives (“We’ll be watching you…. Don’t pull the plug on him, Doc. Don’t you dare”); and the frustrations of a system stretched beyond the point at which it can operate safely (for example, missing radiographs: “I have complained to the chief of radiology, screamed at file clerks, and thrown fits in the reading room. Nothing has ever worked; now I just shrug—beaten by the system—and do what I can without the film”).
Advertisement
He also opens the usually closed issue of iatrogenesis—that is, illnesses caused by medical examination or treatment. Mistakes are common in medicine. A recently published American Institute of Medicine report7 estimated that as many as 98,000 Americans die each year from medical errors. The report argues that mistakes are so common that a Center for Patient Safety should be created to collect information about medical error. The US government’s response to this study has been uncommonly brisk. On February 21, President Clinton endorsed the report’s goal of cutting mistakes by half over five years.8
Murray describes several instances of iatrogenic illness during his month on ICU. One man was given intravenous penicillin, to which he was allergic. Astonishingly, he was given the same antibiotic again during the same admission, which gave him a ticket that took him immediately to the ICU. In another case, a woman with pneumonia was pushed into pulmonary edema—a condition in which the lungs fill with water—by overzealous infusions of intravenous fluids. Murray reports twelve cases of iatrogenic pulmonary edema during his month, and he rails at the “careless physicians” who paid too little attention to preventing this serious complication.
Part of the difficulty, Murray argues, is that doctors have come to rely too heavily on laboratory tests and radiographs to make diagnoses and to monitor treatments. The skills of history- taking and careful physical examination are not endowed with the mystique of a new and expensive technical investigation. And so they are neglected. Murray’s belief in the centrality of these old-fashioned values is confirmed by reading his textbook. In this multiauthored treatise, the chapter on history and physical examination was written by Murray alone. There he affirms the importance of a doctor’s communication skills, which form “the foundation for the physician-patient relationship.” But he also argues that “communication is not just words but is an interaction with sequences and quality.” These subtle transitions between doctor and patient are vital influences “on subsequent trust, understanding, concern, and compliance.”
It follows, therefore, that the medical interview, which is nearly always the first event in the continuum of physician-patient communication and which is the most frequently used tool in clinical medicine, has considerable effect on the outcome of the patient’s illness.
A reliance on technology can make doctors overconfident or, worse, plain lazy. Murray gives an example of how the discovery, by computed tomography, of “free air” in a patient’s abdomen almost led to a major operation to locate a presumed rupture of an internal organ. And yet a thorough clinical examination revealed the “free air” finding to be a red herring. The radiologist, confronted with the negative clinical examination but clinging to his X-ray proof, began to lose touch with reality. “It doesn’t matter what your examination shows,” he exclaimed. “That’s free air, take my word for it.” It was not, and Murray sums up his views about this incident. He is scathing:
…A CT [scan] of his abdomen, which was probably not indicated in the first place, revealed a “finding” that I decided not to act on, but that could have sent him to the operating room. In addition, the turmoil of going to the x-ray department for the CT study in the early morning, when he would have been better off sleeping, and the multiple examinations to resolve the debate, have only served to make poor Mr. McVicker much more terrified and confused than he already was.
These unusually frank reflections raise the question why Murray has written this critical account of ICU medicine. His experiences have led him to ask two large questions. First, is there any point in having an ICU when patients’ outcomes seem so poor? And second, given that the ICU is a place where people frequently die, have we paid enough attention to how they die? His answers to both questions are not wholly reassuring.
2.
A plainly distressed first-year resident challenged Murray directly. “This is my second month at ‘The General’ and almost all my patients have been losers. In the ICU alone, of my five patients, three were drunks and two were junkies…. They’re all trying to kill themselves. What’s the point? Why are we doing this?”
Her observations will ring true for many doctors. And Murray, although he tries to quell her skepticism with a passionate speech about “commitment,” “victims of social bad luck,” and the occasional “brilliant success,” shares some of her doubts. Drug users are, he concludes, “notoriously bad at complying with therapy.” After one patient suffered a huge stroke as a complication of injecting drugs, Murray cannot refrain from remarking: “It is incomprehensible to me how this young man—or anyone—could wreak such destruction on his own body. Yet it happens over and over again.” Add to drug abuse the effects of alcohol and smoking and one has the holy trinity of self-harm. ICU does nothing to tackle these root causes of acute illness.
Murray’s verdict on his month’s work—the real answer to his resident’s question—can be inferred from his stark summary of the outcomes among his sixty admissions—twenty-seven alcoholics and drug users patched up, in all likelihood, only to return again soon, but in ever worsening shape; eighteen episodes of iatrogenic disease; fifteen deaths; nine “notable failures”; and two patients who survived but who now have irreversible brain damage. There were only seven “gratifying rescues,” at a total monthly ICU cost of $1.15 million. Murray asks bluntly whether such “huge expenditures” can be justified.
Physicians use what they call the f-word to describe these situations—futility. Clinical judgment about how to manage the ruinously ill is reduced to estimating a probability: What is the chance of a given intervention achieving a particular goal? Below a certain threshold that intervention is pronounced futile and is thus deemed pointless. Such brutal rationalism may seem fair. But it is almost impossible to put into practice.
Who defines, for example, the threshold of probability? Must the chance of success be better than one in two, one in four, or one in ten? Who decides? How does one calculate a probability reliably and accurately? Murray points out how difficult it is to pinpoint the moment when an illness crosses “the invisible threshold from potentially curable…to hopeless.” And what should the final goal of treatment be? The purpose of the ICU is to preserve life, to restore the patient to near normal functional capacity, and to limit morbidity. But the aims of intervening may be more modest and yet equally reasonable. Murray describes an instance in which he kept a patient peacefully alive to allow the family to come to terms with an approaching death. The purpose of intervention shifted, humanely, from patient to family. These value judgments force decisions about what is futile to be made jointly among the patient, family, and medical team. There is no precise calculus that can be appealed to, and decisions can rarely be extrapolated from one setting to another.
There is an additional problem. The concept of futility is often confused with rationing, and Murray sometimes seems to conflate the two. The cost of ICU medicine is high. To husband limited resources more effectively, one might ask how much we are willing to spend on intensive treatments. But the issue of equitable resource allocation between critical and noncritical care is not equivalent to guessing when a chance of treatment is worth taking or not. These are entirely separate issues. To mix cash flow so intimately with clinical decision-making risks a dangerous ethical shortcut.
In any case, such theorizing may ignore the reality at the bedside. If it was your son, daughter, mother, or father lying in an ICU bed, could you make a rational judgment about the probable outcome? My guess is no. You are more likely to want everything done that reasonably could be done in the absence of undue suffering, even if, when one examined the evidence and weighed the probabilities, the outlook was poor. A probability is, after all, only a probability. Your case could be the one that beats the odds.
Is there a way out of this apparent impasse between a desire to do all one can and making a decision based on probable outcomes? The impediment to answering this question is that, even today, the ICU is an obscure “black box” within the hospital. Cory Franklin, the respected Chicago expert on intensive care, wrote in 1998 that the ICU is
an intricate assemblage of high-tech equipment where patients enter as “input variables” at one end and emerge sometime later from the other end as “outcomes.” Tellingly, unless they have specific business there, outsiders tend to avoid venturing into the ICU. Medical students, residents, and consultants from other disciplines often speak of doing training rotations or visiting the ICU simply to find out exactly what goes on there.9
Murray succeeds in demystifying the ICU by telling its story. But one can also turn to research for answers. In an effort to devise ways of predicting a patient’s outcome, several models for calculating risk have been tested. The best studied is the Acute Physiology and Chronic Health Evaluation (APACHE), first introduced in 1981 and now in its third revision. Risk is calculated according to the patient’s physiological status, age, and pre-existing health. To these variables are added predictive equations reflecting the diagnosis and a large database of additional clinical information. Although these models have identified important aspects of a patient’s physiological state that confer poor prognosis, they are used mainly for research and their place in everyday patient care remains undecided. APACHE III is not a reliable way to differentiate survivors from nonsurvivors.
Yet there is an urgent need for some means of evaluating intensive care. Murray himself deplores “the impossibility of ever knowing whether each of the many decisions I make is right or wrong.” The hope is that explicit approaches to the calculation of risk will enable the work of ICU physicians to be assessed fairly and outcomes to be defined as accurately as possible. This transparency in setting goals might reduce the desire of all parties to embark on a course of futile treatment.
The motive for seeking intervention in dire circumstances can be fostered by mistrust, confusion, and ignorance. Laying out for discussion the factors that are likely to govern an individual’s outlook should lessen all three of these threats to compassionate and appropriate care. But the truth is that all such decisions are going to be imprecise judgments. After twenty years of trying to use the methods of science to answer these impenetrably human questions, I get the sense that many doctors now accept that the best we can do is to do our best. The prop of spurious statistics is at last being discarded.10
3.
In 1821, William Hazlitt reflected on the very issue that Murray draws our attention to at the end of his diary, an issue that causes more angry struggle today than any other in the swamps of modern medical ethics:
It has been thought by some that life is like the exploring of a passage that grows narrower and darker the farther we advance, without a possibility of ever turning back, and where we are stifled for want of breath at last. For myself, I do not complain of the greater thickness of the atmosphere as I approach the narrow house…. I should like to have some friendly hand to consign me to the grave. On these conditions I am ready, if not willing, to depart. I could then write on my tomb—GRATEFUL AND CONTENTED.11
Whose friendly hand should do the consigning remains disputed, and it is a question that certainly perplexes Murray. Of one patient whose life was lost, he notes that “what distressed me was that there was no room in our system for me to leave her alone and let her die peacefully. I was obliged by the rules to intervene.” He writes that these efforts sometimes seem like inducing “a long period of torture” and that “dying in increments with a tube in your windpipe and another in your chest is infinitely miserable.”
A friendly hand can be gripped more tightly or less. The lightest touch is the DNR—do not resuscitate—order that prevents futile clinical intervention if a patient has a potentially fatal crisis, such as a respiratory arrest. In England, we are now in the throes of a critical reexamination of the DNR notice. For years doctors have written DNR orders on patients’ case notes without their consent or knowledge. When a woman with cancer recently survived her ordeal and examined her hospital notes she discovered with horror her medical team’s decision to deny her resuscitation should she require it. She had not been consulted about her intended fate and her case has reignited issues of patient autonomy, medical paternalism, and clinical futility, which the British still seem to have great difficulty confronting.
A physician can take a slightly firmer hold if there is an advance directive to turn to. Murray and his wife both have “living wills,” and those who possess such documents can prevent a hopeless endeavor to repair the irreparable. While advance directives deserve to be encouraged—the 1991 American Patient Self-Determination Act obliges US health care providers to offer patients written information about living wills—they do not, as yet, provide a solution to the puzzle of when to accept the inevitability of death and withhold or withdraw treatment. Just too few patients (Murray cites a figure of around 15 percent) have created advance directives; their doctors may be unaware that such an instruction exists; and there is some evidence that, in any case, advance directives may have only a limited impact on decision-making in the end-of-life setting.
All of which leads to Murray’s final argument, which he lays out briefly in an epilogue. His long working experience of the ICU has led him to believe that a proportion of his present patients should have been offered one of “the many infinitely more humane alternatives to ICU care.” He raises, but never tries to answer, questions of physician-assisted suicide and eutha-nasia. His tone suggests that he is out of sympathy with advocates of either solution to fatal illness. “Doctors are,” he writes, “invariably less enthusiastic than the general public about their would-be role as executioners.”
Still, he acknowledges that this professional mood may be starting to shift. Surveys indicate that more doctors now seem willing to contemplate assisted suicide.12 And he agrees that the evidence from Oregon, where a 1997 Death with Dignity Act legalized physician-assisted suicide within narrowly proscribed rules, seems to suggest that such a law can be implemented without ushering in mass medical slaughter. Importantly,
Contrary to the fears of some, there was no indication that physician-assisted suicide was disproportionately chosen by or forced on terminally ill patients who were poor, uneducated, uninsured, or worried about financial loss.
Further experience of Oregon’s statute shows that only one in six requests for physician-assisted suicide was being granted.13 Crucially, although a fifth of patients requesting assistance committing suicide were clinically depressed, none with treatable symptoms received a lethal prescription. Findings such as these strengthen the argument that assisted suicide can be practiced free from abuse.
But I sense that Murray remains reluctant to allow the physician to cross a line from a position of withdrawing treatment and providing only symptomatic relief to one of actively prescribing drugs to end life. When challenged by a medical student about the care of a man with terminal lung disease and brain damage, he affirms his intention to “give him morphine and allow him to die peacefully. Without the intense terror and agonizing distress of progressive asphyxia.” The bold student tells him that his action would be tantamount to “physician-assisted execution.” Murray demurs, arguing that “the key point is that our intent is to relieve Mr. Caughey’s suffering, not to cause his death, although I agree with you that morphine may quicken it.” These distinctions may seem slight, and they are often rejected as spurious by advocates of physician-assisted suicide,14 but for many doctors, including myself, the difference between an intention to diminish symptoms of suffering and an intention to kill means a great deal.
Murray’s point is that we should take these decisions out of the crucible of technological excess either by not sending patients who are “irrefutably doomed to die” to the ICU or by removing them from the ICU once it becomes clear that a fatal outcome is imminent. There are more humane places—home or hospice, for example—for these patients to go. To some degree, Murray’s pleas are already being heeded. In American ICUs that train critical care specialists, a third of patients who died had life support withdrawn, and a tenth had life support withheld. Only 23 percent had full ICU care, including attempts at resuscitation.15 Although there was variation in practice between ICUs, limits to care are now accepted and commonplace.
There is an omission in Murray’s argument, however, which ultimately distorts the choices he presents. He does not provide a more nuanced discussion of end-of-life care. It is here that substantial conceptual and clinical advances have been made to remove the agony encountered by some patients on ICUs and to draw back from what is beginning to be seen as the far from straightforward practice of physician-assisted suicide.
End-of-life care is poorly taught, if taught at all, to American and British medical students, and almost nothing is included in standard medical textbooks recommended to students either before or after graduation.16 And yet a great deal of research has been done to understand exactly what “end-of-life care” means. The American physician Marion Danis, for example, has brought together doctors who work in intensive care and palliative medicine, experts in medical ethics and education, and consumer advocates to set reasonable professional goals for managing the end of a person’s life.17 They emphasize that care, agreed on jointly with patient or surrogate, must guide technology and not vice versa. (Murray gives several examples of technological imperatives governing care.) Clear decisions about treatment withholding and withdrawal must be made; trust among those taking part in these decisions, based on honest discussion, even in the face of paralyzing uncertainty, should underpin all end-of-life care; cultural diversity must be respected; and the principles of relieving pain and making people more comfortable—palliative care—should occupy a central place in the ICU.
There is a gap, however, between the wishes of professionals and those of patients. When patients are asked what they conceive to be high-quality end-of-life care, the committee jargon of consensus panels is shed in favor of humbling clarity. Patients wish for good measures to relieve pain and symptoms; an end to unnecessary prolongation of dying; a sense of control over their destiny; relief of the burden of physical care and decision-making that rests on family members or friends; and strengthening of relationships with the people closest to them.18 These contrasting views show that physicians prefer to select only aims they can quantify or qualities they can measure, few of which may be uppermost in their patients’ minds.
These matters now demand renewed scrutiny. The hope that assisted suicide might offer a solution to the problem of undignified and costly end-of-life care has recently been proven to be illusory. The Oregon experience, after two years, showed that twelve of twenty-nine patients given supposedly lethal medications did not die. Eleven subsequently died of other causes, and one was still alive when the research was conducted. The conclusion must be that physician-assisted suicide often fails. There are likely damaging physical and psychological consequences of that failure for patients, their families, and the health care team. It is a pity that these compli-cations of unexpected failure were not anticipated by the Oregon researchers.
Worse still, experience from the Netherlands, the country with the most mature system for provision of assisted suicide and euthanasia services, indicates serious unforeseen adverse effects.19 With 15 percent of patients undergoing physician-assisted suicide, there were “problems with completion,” meaning that there was a longer than acceptable time between giving the lethal drug and death. Two patients woke up from their “terminal” coma. For 10 percent of patients, there were technical impediments to assisted suicide, such as difficulties in finding a vein to inject the drug or difficulties with giving drugs by mouth, such as irritation to the throat. And 7 percent of patients experienced complications, including nausea, vomiting, “extreme gasping,” and muscle spasms. The brutal reality of physician-assisted suicide is that it can frequently diminish the quality of end-of-life care, not enhance it.
There is no quick fix to alleviate suffering at the end of life. The challenges for people giving health care are formidable. And yet when palliative measures are offered—effective pain control, a hospice referral, or treatment for depression—almost half of patients who originally seek assisted suicide change their minds.20 And when medical personnel know that palliative care services are available, their early willingness to give a lethal drug seems to diminish.21 Before the public debate about who should receive intensive care, what constitutes medical futility, and what place physician-assisted suicide might have in either setting goes any further, the end of a person’s life deserves a less reductive analysis by physicians and philosophers and the public alike.
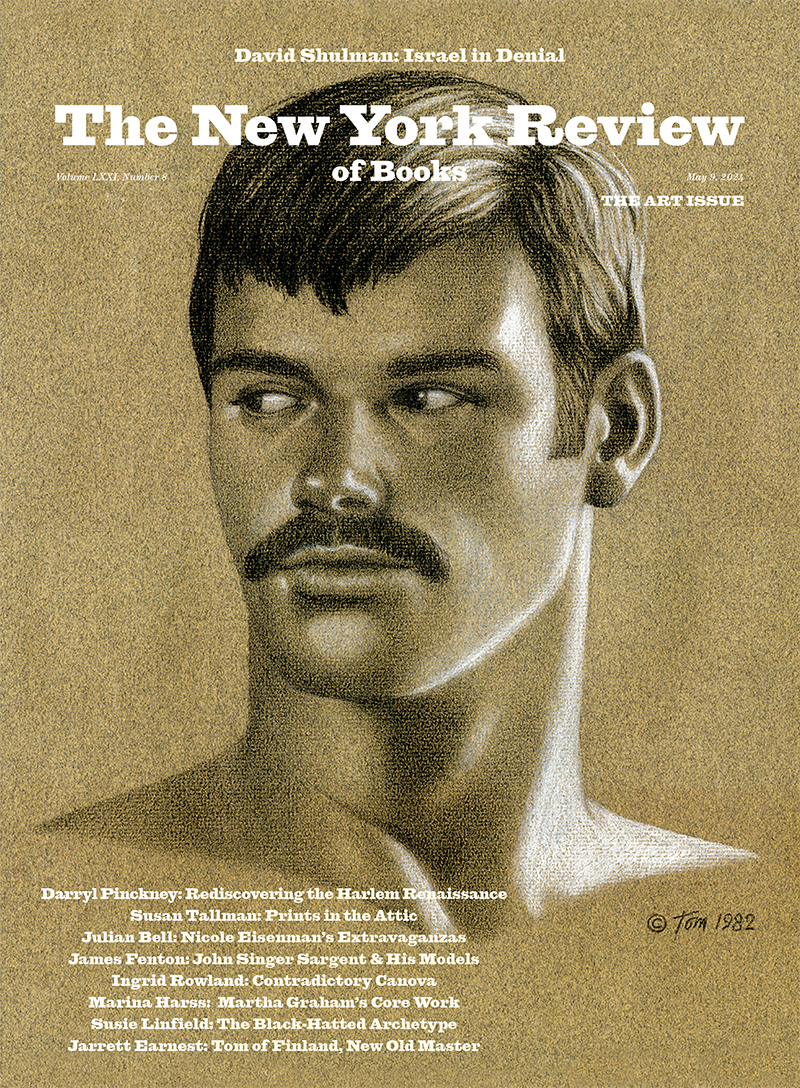
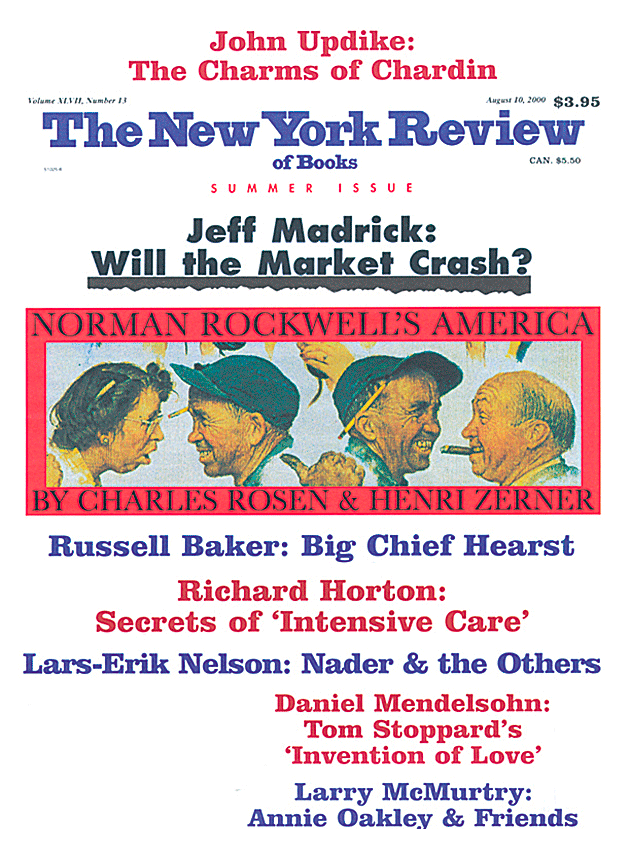
This Issue
August 10, 2000
-
1
Murray conveys this drama by repeatedly using war metaphors. The trauma service is “battle-ready”; despite considerable efforts, his team had “not won the war”; the ICU gets “bombed” with new admissions; a treatment plan is a “full-bore attack”; and antibiotics are “broad firepower” or “big guns.” These commonly used images do give a sense of the sometimes desperate atmosphere of an ICU. They also show, perhaps, the swashbuckling approach doctors take to this most acute of medical specialties. ↩
-
2
New Directions, 1984. ↩
-
3
Both Harcourt Brace, 1996. A new selection of Selzer’s medical essays, including two new pieces, has recently been published (The Doctor Stories, Picador, 1998). The book contains Selzer’s own account of his literary development as a doctor. ↩
-
4
University of California Press, 1999. ↩
-
5
See Kathryn Montgomery Hunter, Doctors’ Stories: The Narrative Structure of Medical Knowledge (Princeton University Press, 1991); and Trisha Greenhalgh and Brian Hurwitz, editors, Narrative Based Medicine (BMJ Books, 1998). The journal Literature and Medicine, published semiannually, aims to report original research in the medical humanities. ↩
-
6
See John F. Murray and Jay A. Nadel, Textbook of Respiratory Medicine (W.B. Saunders, 1994). Intriguingly, Murray’s literary interests are apparent in this treatise. Murray’s wife is the writer Diane Johnson, and she, together with Judy Nadel, wrote in a foreword that the work of textbook authors “had much similarity to a work of fiction,” since “their idea was of course to bring order and reassurance to the turbulent field of pulmonary medicine, rather as a novelist attempts to bring meaningful order to the chaotic events of reality.” I doubt that any fear-some three-thousand-page, two-volume medical textbook has ever received such a generous introduction. ↩
-
7
See Linda T. Kohn, Janet M. Corrigan, and Molla S. Donaldson, editors, To Err Is Human: Building a Safer Health System (National Academy Press, 1999). ↩
-
8
See Robert Pear, “Clinton to Order Step to Reduce Medical Mistakes,” The New York Times, February 22, 2000, p. A1. ↩
-
9
See Cory M. Franklin, “Deconstructing the Black Box Known as the Intensive Care Unit,” Critical Care Medicine, Vol. 26, No. 8 (1998), pp. 1300-1301. ↩
-
10
A breach in the scientistic approach to medical futility was perhaps best expressed in a report from the American Medical Association last year. See “Medical Futility in End-of-Life Care,” Journal of the American Medical Association, Vol. 281, No. 10 (1999), pp. 937-941. ↩
-
11
See William Hazlitt, “On the Fear of Death,” in Selected Writings (Penguin, 1982). ↩
-
12
And not only doctors. In a recent study, two thirds of sampled US medical students supported legalization of physician-assisted suicide and over half said that “they might be willing to assist a patient by writing a lethal prescription.” See Richard S. Mangus et al., “Medical Students’ Attitudes Toward Physician-Assisted Suicide,” Journal of the American Medical Association, Vol. 282, No. 21 (1999), pp. 2080-2081. ↩
-
13
See Linda Ganzini et al., “Physicians’ Experiences with the Oregon Death with Dignity Act,” New England Journal of Medicine, Vol. 342, No. 8 (2000), pp. 557-563. ↩
-
14
Ronald Dworkin has been the most persuasive critic of those of us who might cling to these distinctions. See Ronald Dworkin et al., “Assisted Suicide: The Philosophers’ Brief,” The New York Review, March 27, 1997, pp. 41-47. ↩
-
15
See Thomas J. Prendergast et al., “A National Survey of End-of-Life Care for Critically Ill Patients,” American Journal of Respiratory and Critical Care Medicine, Vol. 158 (1998), pp. 1163-1167. ↩
-
16
Murray and Nadel’s textbook is an unusual exception, since they include a chapter on “Ethics and Withdrawal of Life Support.” ↩
-
17
See Marion Danis et al., “Incorporating Palliative Care into Critical Care Education: Principles, Challenges, and Opportunities,” Critical Care Medicine, Vol. 27, No. 9 (1999), pp. 2005-2013. ↩
-
18
See Peter A. Singer et al., “Quality End-of-Life Care: Patients’ Perspectives,” Journal of the American Medical Association, Vol. 281, No. 2 (1999), pp. 163-168. ↩
-
19
See Johanna H. Groenewoud et al., “Clinical Problems with the Performance of Euthanasia and Physician-Assisted Suicide in the Netherlands,” New England Journal of Medicine, Vol. 342, No. 8 (2000), pp. 551-556. ↩
-
20
See Ganzini et al., “Physicians’ Experiences with the Oregon Death with Dignity Act.” ↩
-
21
See Mangus et al., “Medical Students’ Attitudes.” ↩