The life of Ignác Semmelweis (1818– 1865) is a puzzle that admits no solution. Here was a man whose painstaking investigations, while he was still only in his twenties, led him to devise a means to control the devastating epidemic of childbed fever then sweeping Europe. Semmelweis saved the lives of countless women and their newborn children. He showed how a statistical approach to the problems of medicine could demolish popular but mystical theories of disease. His work prepared the way for Pasteur’s elucidation of germ theory. He turned obstetrics into a respectable science. And he revealed how professional eminence and authority could breed crass stupidity and bitter jealousy.
Yet this Hungarian émigré died in Vienna broken and alone, abandoned by his family and his colleagues in a Viennese lunatic asylum. It took forty years for him to be commemorated in Pest, his home city. The controversy circling his life continued into the 1960s, when his remains were exhumed, reexamined, and finally returned to his homeland. Even today, Semmelweis scholars are partisan. Was Semmelweis the author of his own destruction, the Fool of Pest, as he was called? Or was he the victim of a deliberate character assassination by a racist, anti-Semitic, anti-scientific, decadent, and murderous medical establishment reigning in nineteenth-century Austria?
1.
Semmelweis was the fourth son of a successful Jewish grocer. His schooling, in both Hungarian and German, left him with a hatred of writing, which was to cost him dearly in later years. He began studying law but quickly switched to medicine, completing his degree in 1844 and becoming accredited in midwifery, or the delivery of newborn babies, the same year. At that time, Vienna’s Allgemeines Krankenhaus was the world’s largest and most famous hospital. It housed two obstetric clinics, the first for teaching medical students, the second for training midwives. By 1846, Semmelweis had been appointed assistant to the director of the First Obstetrical Clinic.
Childbed (or puerperal) fever is an acute illness that affects women during labor. It can be aggressively infectious. During a twenty-month epidemic beginning in 1821, for example, childbed fever killed one in six women admit-ted to Viennese hospitals in labor. No one knew the cause. A commonly believed theory blamed noxious airs; as a result there was much drilling of holes through hospital walls and doors in the desperate attempt to improve ventilation. Even in 1864 an expensive ventilation system was being installed in the Viennese maternity clinic. Air ducts were piped through ceilings; iron gratings were laid across corridors. All to no avail.
Semmelweis was quick to notice that the women’s mortality rate in the clinic for medical students was exactly three times that in the clinic for midwives. Between 1841 and 1846, he calculated that 1,989 women died in the company of medical students, out of 20,042 admissions—9.9 percent. The comparable figures for midwives were 691 deaths out of 17,791 hospital confinements—3.3 percent. Women entering the Allgemeines Krankenhaus were only too well aware of these differences. Those admitted to the first clinic begged—“wringing their hands,” according to Semmelweis—to be transferred to the second. Giving birth on the streets of Vienna was safer than within the walls of the city’s most prestigious medical center.
Semmelweis correlated the soaring incidence of childbed fever with the introduction of autopsies into the hospital during the 1820s. When his friend Jakob Kolletschka, a professor of forensic medicine, died from a disease indistinguishable from that of women with fatal puerperal fever, Semmelweis became convinced that somehow cleanliness was at the root of the problem. Kolletschka had cut himself with a knife while conducting an autopsy. Semmelweis suggested that particles from the cadaver must have been transferred into Kolletschka’s bloodstream, thereby causing his death. Medical students were exposed to the same particles from cadavers while performing autopsies. The students could have been a source for the disease that soon overtook the women they went on to care for.
Semmelweis tested his idea by introducing new rules for hygiene in May 1847. He made it mandatory for doctors and students to wash their hands with warm soap and water, to scrub their nails, and to rinse their hands with a chlorine solution until they were slippery. By June, death rates had plummeted to only a few percent. They fell still further when Semmelweis realized that transmission of particles from cadavers could take place from one woman to another. He could stop the fever in its tracks as it moved through a ward by simply insisting on chlorine disinfection of a doctor’s hands after the examination of each woman. His terrifying conclusion was that doctors and their medical students had caused an entirely unnecessary epidemic of deaths. The uterus after birth had to be seen as a huge fresh wound. Only obsessional hygiene could prevent it from becoming a portal for fatal particles introduced through contaminated vaginal examinations.
Advertisement
These were striking and convincing results. But Semmelweis, for reasons that are still a matter of dispute, did not write up his findings for publication. Instead, he left it to colleagues and friends to circulate his discovery. Ferdinand von Hebra was editor of the Journal of the Medical Society of Vienna and he published accounts of Semmelweis’s work in December 1847 and April 1848, inviting others to try out his chlorine disinfection technique. And Charles Routh, who had been a student of Semmelweis’s at the time of his discovery, gave a report of events in Vienna to the Royal Medical and Chirurgical Society on November 21, 1848,1 writing that
the real cause of the mortality from puerperal fever there, was the “uncleanliness of medical men and students in attendance”; their hands being impregnated with cadaveric matter through dissecting, making autopsies, and performing obstetric operations on dead bodies. Dr. Semelweiss recommended all students attending his division of the Lying-in Hospital not to handle dead matter, or, if they did so, forbad them to make any examinations of the patients till the following day. And he directed every student to wash his hands in a solution of chlorine prior to and after every examination made on the living subject. The result was, that the number of deaths was reduced from thirty per month, to seven per month, the usual average mortality of the division for midwives only.2
While his remarkable observations were known to a small circle of close colleagues, Semmelweis’s reputation suffered in the salons of Viennese medicine. Europe had plunged into a period of mid-century chaos, and the revolutions of 1848 divided the Viennese academy as they divided the city’s streets. In March, Prince Clemens von Metternich, a leading advocate of the rights of kings and emperors, threw out democratic reform proposals, enraging students and younger faculty members who were sympathetic to change. This scholarly group of dissidents created an Academic Legion to exert further pressure on the government. Semmelweis was an enthusiastic supporter of the legion, wearing its uniform of plumed hat, gray trousers, and black jacket while giving lectures. Such revolutionary zeal angered the hospital’s old guard, and especially the reactionary head of Semmelweis’s department.
Johann Klein was one man among many who, as the German surgeon Theodor Billroth once noted, had “been reared in an intellectual strait-jacket with dark spectacles before their eyes and cotton wool in their ears.” He rejected Semmelweis’s arguments concerning cleanliness. Along with his colleagues, he probably felt angry that this precocious Hungarian was making orthodox practices—and practitioners—look not only ridiculous, but also dangerous. Indeed, as Sherwin Nuland points out in The Doctors’ Plague, it was Klein who had insisted that medical students examine cadavers in the first place, and it was he who had relaxed constraints on conducting vaginal examinations during labor. Semmelweis seemed to be saying that Klein’s policies were the direct cause of the epidemic.
When Semmelweis’s temporary appointment came up for renewal in March 1849, Klein blocked his application, despite appeals from senior medical colleagues, such as the celebrated pathologist Karl von Rokitansky and the skilled diagnostician Josef Skoda. Semmelweis was even unable to establish himself as an independent physician with the right to admit patients to a hospital. Eventually, and rather grudgingly, he was granted the status of a Privatdozent; but he was unpaid and had to accept the ludicrous understanding that he could only teach students by using a mannequin. Hurt and insulted, he left Vienna for Hungary without even telling his friends or supporters.
Pest was little better. His parents were dead, most of his family were refugees, and he returned to find only his sister and one brother, a Catholic priest, who had converted from Judaism. The academic standards at the University of Pest were low. In May 1851, he was given a second chance. He took an unpaid position in the obstetric division of St. Rochus Hospital in Pest, where he once again introduced chlorine disinfection—with dramatically successful results. His work earned him the chair in theoretical and practical midwifery in 1855, when he was thirty-seven. His life seemed to be settling at last. He married the twenty-one-year-old Maria Wiedenhoffer and, in 1858, published his first paper describing his work in a Hungarian medical journal.
But again he aroused conflict. Opposition to his work seemed to be growing stronger. For reasons that still remain obscure, the great Viennese pathologist Rudolf Virchow denounced Semmelweis. And amid these unpleasant arguments, Semmelweis began writing the book that would finally destroy as well as make his reputation.
The Aetiology, the Concept, and the Prophylaxis of Childbed Fever was published in 1861. It is divided into two parts. In the first, Semmelweis assembles a vast collection of data, presented in sixty-three detailed tables, to construct a theory for the transmission of puerperal fever. In addition to his observations among women, he included results from experiments on rabbits, which lent support to his view that particles deriving from autopsies provided the source of disease. It is a dense treatise, but one that bears witness to the remarkable thoroughness with which he conducted his investigations. The second part attacks his critics. He wrote that the medical students under his care knew enough about modern obstetrics to “laugh Virchow to scorn.” He criticizes Carl Braun—who succeeded Semmelweis at the Allgemeines Krankenhaus and then went on to take up Johann Klein’s professorship upon Klein’s retirement—for his lack of basic logic. And he called Friedrich Scanzoni, the professor of obstetrics in Würzburg who had been skeptical about his theories, a “wretched observer” of his discoveries.
Advertisement
The book, while it collected all of Semmelweis’s investigations for the first time in one volume, met with harsh reviews—and with dreadful results for medical care. For even in 1861, puerperal fever was an ever-present threat. At a meeting of the Obstetrical Society of London, for example, Dr. W. Tilbury Fox reported the “very high death rate” from puerperal fever between 1833 and 1858, over 3 percent.3 In the debate that followed, even the greatest obstetricians of London had to admit they “did not know what puerperal fever really was.” Standard treatment at the time included bleeding, leeching, and mercury. The president of the society proclaimed that “the obstetrist could put before him no nobler object than the diminution of this mortality.”
But Semmelweis’s Aetiology was a balanced treatise compared with the accusing open letters he circulated, which Nuland has previously translated in collaboration with Ferenc Gyorgyey. He taunted Scanzoni for sending
out a significant contingent of unwitting murderers [his students] into Germany…. I declare before God and the world that you are a murderer and the “History of Childbed Fever” would not be unjust to you if it memorialized you as a medical Nero, in payment for having been the first to set himself against my life-saving theory.
His poor judgment and erratic behavior only got worse. Semmelweis roamed the streets of Budapest muttering to himself and distributing pamphlets directed against those who refused to follow his teachings. He seemed to swing from periods of excitement and energy to paralyzed depression. By July 1865, he appeared to be deranged. On July 21, at a regular gathering of the Pest college of professors, Semmelweis was invited to speak about a vacancy for a lecturer’s position in his department. According to one account, he rose and quite unexpectedly began reading the midwives’ oath. A week later, his wife had him committed to psychiatric care—incarceration in a brutal asylum would be a more accurate description. He died on August 13, aged forty-seven.
The long-held view was that Semmelweis died from a bacterial infection of the blood, sustained after a cut to his finger, a sadly ironic result in view of his work with puerperal fever. But the excavation of his remains in 1963, together with the discovery of new documents in the 1970s, suggests a more tragic end.
It seems that Semmelweis was lured to the Viennese mental asylum by his wife. He thought he was traveling first to a spa in Grafenberg and then to Vienna to visit and work in the house of Ferdinand von Hebra, his longtime friend and advocate. Once he had arrived, three doctors, none of whom was a psychiatrist, approved his involuntary imprisonment in one of Vienna’s nastier institutions. He resisted efforts to constrain him, after which he was put into a straitjacket and locked in a darkened cell, where he was beaten for his recalcitrance. When he died not long after, the medical press simply noted his death, and there were no obituaries recognizing his accomplishments.4
2.
Sherwin Nuland, a professor of surgery at Yale and a historian of medicine, has studied Semmelweis’s life for almost thirty years. In 1979 he provided a radical reinterpretation of the biography of this hitherto much praised physician.5 Using typically colorful language, he described the demise of Semmelweis as fitting the pattern of a Sophocles play—“a hero, a truth, a mission, and finally a flight of passionate arrogance resulting in downfall.” Semmelweis possessed a “fundamental fault” in his character. He had a “self-destroying psyche.”
It could have been so different, Nuland claims. At the time of his discovery of the causes of infection in Vienna, the Austrian medical establishment was shedding its encrusted past and a new generation of scientifically minded physicians was taking over. Rokitansky became rector of the university in 1852. Hebra was editor of an influential journal. Yet when Semmelweis had the chance to explain his work, he said hardly anything. The standard reason given for this silence was his fear that he was vulnerable to attack in view of his background as a Jewish Hungarian who spoke poor German. But if he seemed to have a touching humility, Nuland writes, he also had a more dangerous trait:
The reality of his genius, of his immense discovery, of his powerful friends, never overcame his greater sense of unworthiness. As in all psychopathology, that self-concept lived side by side with its opposite; a megalomania, a rage, and finally a towering hurricane of grandiosity that swept him to his destruction.
Eventually Semmelweis did speak out. He read a paper to the Medical Society of Vienna in May 1850. He triumphed over his enemies, but again—hubris? laziness? insecurity about the quality of his German?—he refused to publish his arguments. Nuland is dismissive of the claim that Semmelweis had a “bruised soul.” He accuses Semmelweis of cowardice, of precipitously returning to Hungary “because it was safe.” In an earlier article, he makes a cruel analogy—that of a man who
runs back to a mother…. He made himself believe in the fantasy of his rejection because it gave him the rationalization he needed to rush back into that mother’s protecting arms.
But Semmelweis’s mother had died in 1844, and whatever he was returning to in 1850, it was not his mother. He was going back to his homeland after his career had been unfairly destroyed in Vienna.
Nuland’s indictment is remorseless. Semmelweis, he argues, was impetuous. He failed to create a network of colleagues who could act as his advocates. Indeed, he deserted the few friends that he had won over. Opposition was therefore inevitable, all the more so in view of his hot temper and injured pride. His descent into psychosis was rapid.
Nuland’s 1979 article had a powerful effect on Semmelweis studies. The largely respectful way in which this Hungarian obstetrician’s work had been discussed now gave way to unrestrained criticism. Nuland developed his theory still further. In a retelling of the story for a series of medical biographies in 1988,6 he called Semmelweis “obdurate,” “obstinate,” and “stubborn.” Semmelweis displayed failings of character. He was “forcefully obnoxious,” a “hellfire-spewing evangelist,” and a “righteous goad.”
While The Doctors’ Plague relies heavily on these two previous accounts, Nuland has increased the concentration of his critical acid. There is even a flash of Semmelweisian stubbornness in Nuland’s version of history. He describes how his theory about Semmelweis’s death was not, at least at first, universally accepted. But “time has only strengthened” his view and, on the wider perspective of Semmelweis’s life, “my basic arguments are the same as they were then [in 1979], and I feel more strongly than ever that they are valid.” This tone of certainty reminds me of Semmelweis’s own view of himself toward the end of his life. With his original inquiries long-ago completed, Semmelweis aimed only to persuade others of his point of view—in ever more shrill terms. There was no room left for alternative explanations or mitigating arguments.
Nuland criticizes Semmelweis not only for refusing to publish his findings in the conventional academic manner, but also for his lack of scientific rigor. But Semmelweis was not an academic like Rokitansky and Scanzoni. He was a medical practitioner who specialized in obstetrics. He had no advanced scientific training, and no mentor who was close to him—certainly not his superior, Klein. There was nobody to advise him day-to-day in the subtleties of scientific etiquette. Nuland seems to judge his subject according to commonly accepted twenty-first-century rules of medical science. This is unfair. When Nuland blasts Semmelweis for what he did not know—the value of laboratory research, for example—one senses that he is unwilling to take account of the limitations of Semmelweis’s medical education and the setting in which he worked. Nuland sees Semmelweis’s predicament as “largely his own fault,” his fight “lonely because he chose to make it so.”
What is so striking about this uncharitable account is the almost complete lack of empathy and understanding Nuland shows for a man who quite clearly had a serious psychological instability. Nuland has diagnosed Semmelweis as suffering from Alzheimer’s disease. But the mood swings that characterized Semmelweis’s behavior before his final mental collapse could also have resulted from a form of manic-depressive illness. We shall never know for sure. We do know that the last years of Semmelweis’s life were blighted by symptoms of psychosis, symptoms that might have manifested themselves in milder form earlier in his career. Some of the elements of Semmelweis’s illness may already have been present at the time of his discoveries in the late 1840s. If so, he deserves even greater sympathy.
For whatever reasons, Semmelweis was unable to match his discoveries with an appreciation of how best to persuade colleagues of their devastating responsibility for provoking an epidemic. This personal failure does not detract from the obses-sive tenacity with which he pursued his cause. In 1970 the American surgeon Owen Wangensteen argued that it was Semmelweis—and not Britain’s Lord Lister—who should be cred-ited for working out the principle of antisepsis.7
More significantly still, the philosopher and historian Codell Carter, with whom Nuland admits he has “interpretive” disagreements, has argued that Semmelweis was among the first to realize the need for a single cause to explain each episode of puerperal fever.8 Semmelweis anticipated germ theory twenty years before Pasteur explicitly formulated it. In his 1850 lecture, for example, Semmelweis argued that for every woman who fell ill, it would be possible to trace the origin of her disease back to rotting organic animal matter. This was a vital contribution to the theory of puerperal fever, as well as to its practical control.
Carter has published a series of highly original and carefully validated observations about Semmelweis since completing the only modern English translation of the Aetiology in 1983. For instance, he demonstrates that the view that Semmelweis made little effort to communicate his discoveries is quite wrong. In 1847, together with his students, Semmelweis wrote letters to leading obstetricians across Europe describing his findings and inviting replies. One letter by a student, perhaps the earliest known description of Semmelweis’s work, was sent on December 21, 1847, to Professor Gustav Michaelis of Kiel.9 The student described the raging epidemic of puerperal fever in Vienna, which seemed resistant to every kind of intervention. He reported details of Semmelweis’s discovery that the uterus was the disease’s point of origin and that “some harmful substance” was being transmitted, most probably a “corpse infection.” He explained the efficacy of washing with chlorina liquida. The letter ends modestly. Semmelweis’s advocate writes that their findings “deserve attention and may encourage similar experiments in other maternity hospitals.”
Strangely, in view of the enormous interest in Semmelweis, new secrets about his life were still being discovered well into the 1970s. Nuland cites, for example, Georg Silló-Seidl, a Hungarian doctor, who, in 1977, found twelve pages of documents concerning him in the Vienna archives. They revealed for the first time details of Semmelweis’s medical examination immediately before being sent to the asylum, the order sending him there, a medical record of his stay, the plan for his autopsy, and a final diagnosis.10 These papers describe his disturbed state of mind. According to the doctor who examined him, Semmelweis
began to be indifferent to the family…. He sought opportunities to entertain himself elsewhere…. [His drinking] exceeded the limits of moderation…. His behavior became more unseemly…. Those around him have noticed a heightened sexual excitement…. [H]e now established relationships with a prostitute.
Once inside the asylum, he was excited, confused, and restless, speaking loudly, moving unpredictably, screaming occasionally, and entering periods of trembling frenzy. The final entries in the asylum’s diary describe his lonely extinction:
…he took off his clothes[, and] lay down on [the] floor…. He stutters more noticeably…. The right foot is dragged behind during his broad, uncertain walking…. He knows no one…. Lower jaw hanging down somewhat…eyes glassy, half open…. Evening death.
His wife, Maria, did not attend his funeral.
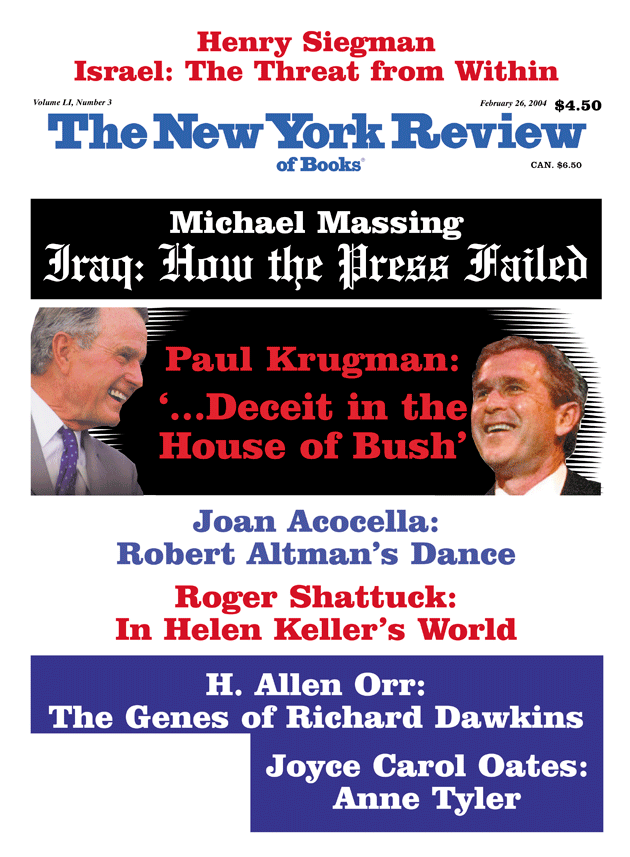
This Issue
February 26, 2004
-
1
See C.H.F. Routh, “On the Causes of the Endemic Puerperal Fever of Vienna,” The Lancet, December 9, 1848, pp. 642–643. ↩
-
2
The reaction to this paper was skeptical. One respondent from the audience criticized Routh for paying insufficient attention to the circumstances in Vienna: “It was well known that Vienna was the most unhealthy place in Europe. Fever of a low type was very prevalent there. The hospital was situated in a damp position, and was ill-ventilated, and unclean. The students, also, were anything but cleanly,” said one D. Webster. ↩
-
3
See W. Tilbury Fox, “On Puerperal Fever,” The Lancet, November 23, 1861, pp. 500–501. ↩
-
4
See British Medical Journal, August 26, 1865, p. 215. His life has, nonetheless, provided inspiration for several writers, Louis-Ferdinand Céline’s doctorial thesis, for example. And the Norwegian Jens Bjørneboe wrote a sympathetic play which premièred in Oslo in 1969, entitled simply Semmelweis. ↩
-
5
See Sherwin B. Nuland, “The Enigma of Semmelweis—an Interpretation,” Journal of the History of Medicine and Allied Science, July 1979, pp. 255–272. ↩
-
6
See Sherwin B. Nuland, “The Germ Theory Before Germs,” in Doctors: The Biography of Medicine (Knopf, 1988), pp. 238–262. ↩
-
7
See Owen H. Wangensteen, “Nineteenth Century Wound Management of the Parturient Uterus and Compound Fracture: The Semmelweis–Lister Priority Controversy,” Bulletin of the New York Academy of Medicine, August 1970, pp. 565–596. ↩
-
8
See K. Codell Carter, “Ignaz Semmelweis, Carl Mayrhofer, and the Rise of Germ Theory,” Medical History, Vol. 29 (1985), pp. 33–53. ↩
-
9
See K. Codell Carter and George S. Tate, “The Earliest-Known Account of Semmelweis’s Initiation of Disinfection at Vienna’s Allgemeines Krankenhaus,” Bulletin of the History of Medicine, Vol. 65 (1991), pp. 252–257. ↩
-
10
See K. Codell Carter, Scott Abbott, and James L. Siebach, “Five Documents Relating to the Final Illness and Death of Ignaz Semmelweis,” Bulletin of the History of Medicine, Vol. 69 (1995), pp. 255–270. ↩