I began writing these words on what appeared to be an unremarkable Sunday morning. Shortly before sunrise, the bedroom still dim, I awoke and quietly made my way to the kitchen, careful not to disturb my still-sleeping wife. The dark-roast coffee was retrieved from its place in the pantry, four scoops then placed in a filter. While the coffee was brewing, I picked up The New York Times at the door. Scanning the front page, my eyes rested on an article mentioning Svoboda, the far-right Ukrainian political party (svoboda, means, I remembered, “freedom”).
I prepared an egg-white omelette and toasted two slices of multigrain bread. After a few sips of coffee, fragments of the night’s dream came to mind: I am rushing to take my final examination in college chemistry, but as I enter the amphitheater where the test is given, no one is there. Am I early? Or in the wrong room? The dream was not new to me. It often occurs before I embark on a project, whether it’s an experiment in the laboratory, a drug to be tested in the clinic, or an article to write on memory.
The start of that Sunday morning seems quite mundane. But when we reflect on the manifold manifestations of memory, the mundane becomes marvelous. Memory is operative not only in recalling the meaning of svoboda, knowing who was sleeping with me in bed, and registering my dream as recurrent, but also in rote tasks: navigating the still-dark bedroom, scooping the coffee, using a knife and fork to eat breakfast. Simple activities of life, hardly noticed, reveal memory as a map, clock, and mirror, vital to our sense of place, time, and person.
This role of memory in virtually every activity of our day is put in sharp focus when it is lost. Su Meck, in I Forgot to Remember, pieces together a fascinating tale of life after suffering head trauma as a young mother. A ceiling fan fell and struck her head:
You might wonder how it feels to wake up one morning and not know who you are. I don’t know. The accident didn’t just wipe out all my memories; it hindered me from making new ones for quite some time. I awoke each day to a house full of strangers…. And this wasn’t just a few days. It was weeks before I recognized my boys when they toddled into the room, months before I knew my own telephone number, years before I was able to find my way home from anywhere. I have no more memory of those first several years after the accident than my own kids have of their first years of life.
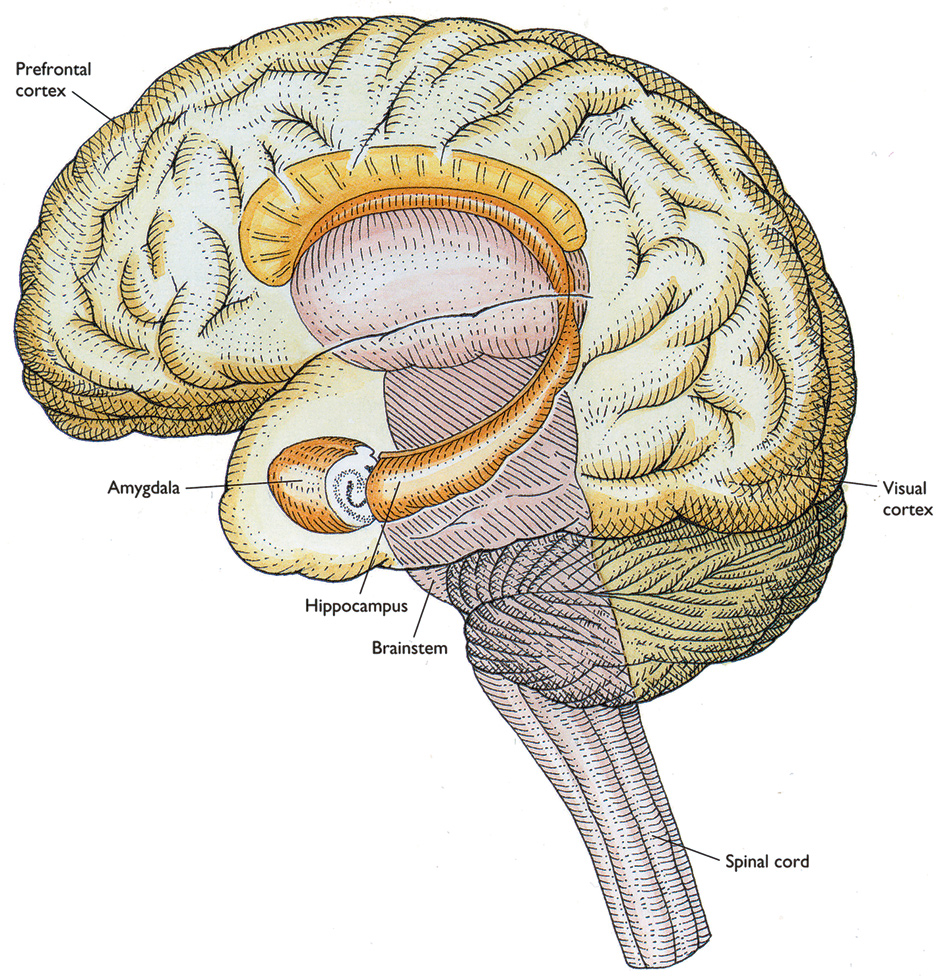
A computed tomography (CT) scan of Meck’s brain showed swelling over the right frontal area. But neurologists were at a loss to explain the genesis of her amnesia. Memory does not exist in a single site or region of the central nervous system. There are estimated to be 10 to 100 billion neurons in the human brain, each neuron making about one thousand connections to other neurons at the junctions termed synapses. Learning, and then storing what we learn through life, involve intricate changes in the nature and number of these trillions of neuronal connections. But memory is made not only via alterations at the synaptic level. It also involves regional remodeling of parts of our cortex. Our brain is constantly changing in its elaborate circuitry and, to some degree, configuration.
Researchers divide memory into categories, the most familiar to us being “declarative,” memory that is consciously recalled. It is the type of memory that was set off by the article in The New York Times. How was my memory of the meaning of svoboda initially acquired and then stored?
I first learned that svoboda means “freedom” in 1988, when I studied Russian prior to a scientific visit to the USSR. Within hours of acquiring that fact there was growth of new synaptic connections between neurons, as well as restructuring of existing synaptic connections, in the part of my brain called the hippocampus (“seahorse” in Greek, due to its shape). These synaptic changes were linked to a series of biochemical changes: release of messenger molecules within the neurons, as well as switching on genes that led to the production of new proteins.
The rapid process of initial memory stabilization in the hippocampus could have been easily disrupted. Perhaps my beeper would have buzzed, alerting me to a medical emergency, diverting my attention away from the new vocabulary. Such diversions can interfere with the biochemical cascade and block new memory formation. Twenty-six years later, I would not have registered the meaning, and thus the irony, of the political party Svoboda.
Advertisement
How was the fact stored? It turns out that our records of life experiences are gradually transformed into a more permanent form in which they are relatively stable. Neuroscientists use the term “consolidation” to describe these post-experience processes of memory stabilization. Consolidation involves reorganization of the brain both at the level of synapses—the connections between nerve cells—and at the level of brain regions. Within hours, consolidation at synapses is complete, with changes in localized neurocircuits. Regional consolidation is a more prolonged process and involves the gradual reorganization of areas of the brain that support memory. Such remodeling occurred not only for the declarative memory that svoboda means “freedom”: it also occurred for the recurring dream that I first had in college, and for the memory that the woman next to me in bed is my wife.
A second category of memory is termed “nondeclarative.” These memories are not conscious but essentially reflexive, yet also involve synaptic changes and reorganization at the regional level. Classical examples include swinging a tennis racket or riding a bike, and on that Sunday using a fork and knife, and deftly scooping coffee.
Neuroscientists have gained considerable insight into memory by studying certain people who have lost it. One such person is known by the initials HM. He suffered from severe epilepsy that could not be controlled with medication. In 1953, his medial temporal lobes, parts of the brain roughly at the level of the sideburns, were removed in an experimental surgery. Although the operation succeeded in reducing the frequency and severity of HM’s seizures, it left his memory profoundly impaired.
Over the ensuing five decades, nearly one hundred studies have been conducted on him, both at the Montreal Neurological Institute and at the Massachusetts Institute of Technology.1 In initial studies, his neurosurgeon, William Beecher Scoville, and the psychologist Brenda Milner observed that HM could not remember articles on the front of the day’s newspaper. This inability to form new memories is called anterograde amnesia.
HM’s deficit included memories not only of new facts (semantic memory) but also of events (episodic memory). Yet he could retain a number or a visual image for a short period of time after learning it. He also remembered events from his childhood. Scoville and Milner posited that the medial temporal lobes were needed to generate recent, but not remote, memories. In later experiments, such long-term memories were discovered to be stored in the cortex, including areas that originally processed the information.
In 1962, Milner conducted a now famous experiment that yielded surprising results: despite all his deficits, HM was able to learn new motor skills. Milner asked HM to trace the outline of a star shown in a mirror. He could see only his hand, because the pencil and star were reflected in the mirror, with left and right reversed. Over the course of several days, HM performed this mirror-tracing task, and on each sequential attempt, he reduced the time it took and made fewer errors. Yet each time he began to trace the star once again, he told Milner that he had never done it before. Though he lacked “declarative memory” (that is, awareness of prior attempts), HM was able to retain his level of improved performance for as long as a year. Milner concluded that such skills, which depend on visual perception and motor ability, appear to involve brain regions outside of the medial temporal lobes.
Two luminaries in the field, Larry R. Squire, at the University of California, San Diego, and the Nobel laureate Eric R. Kandel, at Columbia University, describe these studies on HM in their elegant and engaging book, Memory. Written in accessible language for a lay reader, the authors illustrate fundamental discoveries about memory using works of art. One particularly illuminating reproduction is Black Wall by Louise Nevelson, in which the artist displays whole and fragmented found objects in crates fixed together as a unit. Squire and Kandel find this “reminiscent of the composition of the brain in which separate modules cooperate to support declarative memory.”
My memory of the topography of my home allowed me to exit the bedroom in the dark, walk to the kitchen, and locate the pantry. Topographical memory was remarkably preserved in HM. Twenty-four years after his operation, on a visit to MIT, Suzanne Corkin, a researcher at the Department of Brain and Cognitive Sciences, asked him to draw a floor plan of his former house. He did so successfully.
The understanding of topographical memory was greatly advanced in 1971 when British researchers at University College London discovered that the hippocampus, that seahorse-shaped structure in the brain, can form an internal representation—a cognitive map—of a spatial environment. Our location in space appears to be encoded in the firing pattern of what are called pyramidal cells, specifically the subset of pyramidal cells aptly called place cells. When an animal moves around and enters different regions of a familiar environment, different place cells in the hippocampus fire, providing a moment-to-moment location within the environment.2
Advertisement
Squire and Kandel emphasize that there is still no test that allows one to pinpoint a memory directly in the mammalian brain; we cannot as yet locate the site where memory of some particular object, like my bag of coffee, is stored. Nevertheless, studies of healthy volunteers and patients with brain lesions by means of MRI imaging show that there are brain regions in the cortex involved in the perceiving and processing of color, size, shape, and other object attributes that are close to, if not identical to, the brain regions important for remembering those objects. Remarkably, the molecules that serve as building blocks for memory are highly similar across species, so that snails and fruit flies learn in ways roughly comparable to mammals.
Even though no single memory site exists, memory is not distributed uniformly in the brain. While several regions typically represent a single event, each region contributes uniquely to the whole representation. Neuroscientists call this an engram: what Squire and Kandel refer to as “the sum total of changes in the brain that first encoded an experience and that then constitute the record of that experience.”
Emotion works to enhance memory. We appreciate that emotionally fraught moments, like entering the amphitheater to sit for a final examination, are often readily recalled. Research studies show that subjects who experienced considerable emotional arousal as they heard someone telling a story remembered that fraught part of the narrative better than parts of the tale told in neutral language. Again, patients with disorders helped reveal to researchers that those with lesions in the amygdala, a deep region of the brain associated with fear and anxiety, did not remember the fraught part of the story better than the neutral parts. Thus, the amygdala appears to be an important brain region involved in what is termed emotional memory.3
My efforts to avoid disturbing my wife’s sleep are also relevant to memory.4 Many of us may have noted that we think better after a good night’s sleep. So-called slow wave sleep (SWS) coordinates the reactivation and redistribution of hippocampus-dependent memories to sites in the cortex, while rapid eye movement sleep (REM) appears to facilitate synaptic consolidation of memories in the cortex. These sleep states help transform new and initially changeable memories into a more stable representation that becomes integrated into the network of preexisting long-term memories. Disturbing my wife’s SWS or REM sleep could impair memory formation and the retrieval of facts and events needed the next day in work or social exchanges.
Insight into the biology of memory comes not only from cases like HM, where parts of the brain are removed. In 1972, during his training in neurology at the University of California, San Francisco, Dr. Stanley Prusiner was called to see a new patient. She was sixty years old, from Marin County, a well-tanned, slim woman, sitting calmly on the side of her bed. When Prusiner asked what was wrong, she could not find the words to describe her symptoms.
Her husband reported that over a relatively short period of time, she had developed problems with memory, as well as difficulties putting the key in the car ignition and unzipping the ball component on her golf bag. The patient’s rapid and progressive dementia in conjunction with jerky muscle movements proved to be manifestations of a rare disorder, Creutzfeldt-Jakob disease. The unknown cause of her malady led Prusiner on what he calls in his new book, Madness and Memory, “a scientific odyssey” of discovery.
Clues ultimately came from the work of anthropologists and medical scientists who had identified a degenerative neurological disorder, called Kuru, associated with participation in ritualistic cannibalism in New Guinea. Prusiner explains:
Kuru was confined to the Fore [people] and bordering tribal areas. The largest afflicted group consisted of young women, followed by children of both sexes, but with girls outnumbering boys two to one. The few adult male victims were generally older than the women.
The disease was documented to be infectious in nature, but over the decades no researcher could identify a parasite, bacterium, or virus that accounted for its transmission. Prusiner labored, in his own telling, as a “pariah” in the neurological field; he conducted studies on sheep with a similar syndrome that ultimately indicated that the infectious cause was a protein that had no genetic information in the form of RNA or DNA. This was completely at odds with all prevailing biological dogma, and Prusiner’s work was largely dismissed in the scientific establishment. Ultimately, he was shown to be correct, and came to name the infectious protein a “prion.”
With further research, Creutzfeldt-Jakob disease, the rare malady affecting the woman from Marin County, was linked to Kuru as also caused by a prion. The infectious prion is misshapen, or abnormal in shape, and interacts with normal cellular prion proteins in a chain reaction—normal proteins become misshapen after contact with the abnormal prion, and then go on to infect other normal proteins. For this to happen, the “good guys,” Prusiner writes, “needed to come in contact with the bad ones as new prions formed.” Instead of normal prions aggregating into spiral-like structures (such as alpha helices), the aberrant prions form primarily flat bands of amino acids (beta-sheets). This molecular origami results in accumulation of the abnormal prions in neurons.
The clinical picture of prion diseases can be quite variable, and includes dementia, disturbances of gait (ataxia), insomnia, paraplegia, and deviant behavior. In some cases, on direct examination, the brain shows widespread loss of cells, leaving cavities so that the organ resembles a sponge. This visual impression led to calling prion diseases “spongiform encephalopathies.” The existence of prions was dramatically brought into the public mind with mad cow disease in the United Kingdom, another spongiform encephalopathy. Cases have also occurred among children with short stature who were treated with growth hormone extracted from human pituitaries harvested from cadavers; presumably, abnormal prions were present in the harvested brains. (With the advent of genetic engineering, human growth hormone is now prepared through recombinant DNA technology, free of prions.)
Prusiner has evolved from a “pariah” to a “prophet” and now predicts that prions explain the genesis not only of rare disorders like Kuru and Creutzfeldt-Jakob disease, but also a spectrum of common degenerative diseases of the central nervous system associated with dementia, including
Alzheimer’s, Parkinson’s, Lou Gehrig’s (ALS), and Huntington’s diseases, as well as the frontotemporal dementias (FTDs), including posttraumatic forms called dementia pugilistica and chronic traumatic encephalopathy (CTE).
Prusiner writes:
It took more than a quarter of a century for the prion concept to emerge from the shadows cast by so many confounding observations. But we are now at the point where the burden of proof is beginning to shift from those who claim prions cause such common illnesses as Alzheimer’s and Parkinson’s to those who deny this etiology.
This March, researchers from Rush University Medical Center in Chicago and the University of California, San Francisco, published data from a study of 2,566 people aged sixty-five years or older who had no dementia when the study started. Their risk for developing Alzheimer’s disease over the ensuing ten years was estimated to be more than 35 percent. If this analysis is sound, then more than half a million Americans aged seventy-five years and older succumbed to the malady in 2010. The new study ranked Alzheimer’s disease as the third leading cause of death, after heart disease and cancer.5
Alzheimer’s disease usually begins in one’s sixties and seventies. Initially, short-term memory fades, and then gradually long-term memory, in conjunction with difficulties in cognition, including confusion, disorientation, and poor emotional control. In the last stage of the disease, patients typically lose basic bodily functions, and die of pulmonary infections from aspirating food and saliva.
Alois Alzheimer, a German psychiatrist and pathologist, is credited with first describing the disorder in 1906. He had attended to a middle-aged woman whose cognition and memory became profoundly impaired. At autopsy, Alzheimer observed microscopic deposits in parts of her brain that he termed “plaques.” He also noted so-called “tangles” within neurons. Looking for these changes after the patient has died remains the definitive method to diagnose Alzheimer’s disease, although recent advances in brain imaging utilizing specialized isotopes can also reveal the distinctive plaques.6
These plaques contain the protein beta-amyloid, while the tangles are composed of the tau protein. There is an intense debate about which protein disrupts neural circuits, leading to dementia. The beta-amyloid protein camp, who call themselves “baptists,” contend that plaques disrupt the normal and effective transmission of signals at synapses between neurons, while the “tauists” posit that the tau protein in tangles wreaks havoc by disrupting the interior functions of cells.
While the controversy continues, recent genetic studies bolster the beta-amyloid camp. In the Medellín region of Colombia, the neurologist Francisco Lopera described an extended family that now numbers in the thousands who typically develop dementia by their fourth decade. They all carry a mutated gene for the enzyme that normally cleaves the precursor of the beta-amyloid protein, but does not in this case, so there is accumulation of an elongated form of the protein. The mutation is traced back to a Spanish settler who arrived in Colombia in the 1700s. Brain scans using the specialized isotopes show diffuse deposits of beta-amyloid that begin in these Colombians’ twenties. The elongated protein is deposited most heavily in the hippocampus and those regions of the cortex involved in short-term and long-term memory.
Other recent studies from Iceland have identified individuals with a genetic mutation that can be seen as the converse of the one in Colombia. Here, the mutated DNA reduces the frequency with which the elongated beta-amyloid protein is produced. Such Icelanders appear to enjoy intact cognition into their ninth decade.
As Prusiner posits, a molecular origami of misshapen proteins may be fundamental to the genesis of many neurodegenerative disorders. In Alzheimer’s the misfolded protein is beta-amyloid or tau; in Parkinson’s disease, the protein alpha synuclein clumps together into what are termed Lewy bodies; and Huntington’s disease, an inherited malady that famously struck Woody Guthrie, appears to result from the incorrect folding of a protein called huntingtin. Whether toxic prions participate in such folding, as Prusiner believes, is a matter of debate.
Prusiner further argues that his unifying hypothesis leads to a strategy to prevent or treat such disorders by targeting misshapen proteins. Such an approach is currently being tested in the United States among patients with Alzheimer’s disease who do not have a clear genetic predisposition, and trials will soon begin in the Colombian cohort. In both settings, antibodies that prevent the clumping of elongated beta-amyloid are being evaluated.
Critics of the tight focus of Prusiner and like-minded researchers on misshapen proteins point to the fact that sophisticated brain scans of some healthy individuals with intact cognition and no signs of dementia show heavy accumulation of beta-amyloid, casting doubt on its sole role. Margaret Lock, professor emerita in the Department of Social Studies of Medicine and the Department of Anthropology at McGill University, in The Alzheimer Conundrum, portrays as myopic this “dominant model” of the disease, which makes “no attempt to research variables other than those internal to the brain.” On the contrary, she writes,
It is probably safe to assume that dementia is universally distributed through time and space, but contemporary research, including the emerging work on epigenetics, has made it clear that it is not equally distributed within or among families, communities, or populations, strongly supporting the position that environments—sociopolitical and ecological—influence the development and functioning of the brain.
She asserts that “dimensions that account for the prevalence of these diseases—above all, poverty, inequalities, and the promotion and marketing of fast food” have to be systematically tackled, “something that is beginning to take place in certain towns and cities, such as the restrictions in size of soda bottles suggested by Michael Bloomberg,” the former mayor of New York City.
Lock’s question is a fundamental one in all of medicine: Why do some individuals develop full-blown disease and others do not, despite sharing the same causative agent? For example, there is diversity in the outcome of AIDS after infection with HIV, or liver failure after contracting hepatitis C, among a population carrying the respective virus. There is an intricate interplay of the inciting agent with the specific genetic makeup of the individual, as well as environmental factors that may shape gene expression (“epigenetics”).
The complexity of the three factors is considerable, and of necessity, researchers and clinicians take an initially reductionist approach. The stunning success of antiretroviral drugs in combating the consequences of HIV infection supports such a strategy. If beta-amyloid or tau is the inciting toxic protein, then initial treatment strategies rightly focus on that target. Proof of the effectiveness of this reductionist approach is likely forthcoming from the studies in Colombia of individuals with the mutated gene, who all develop Alzheimer’s disease.
To be sure, there is merit in seeking environmental factors that affect risk for a disorder like Alzheimer’s disease. And many researchers are, in fact, studying this by examining effects of insulin and other metabolic molecules.7 But in this search we need to be alert to wishful thinking. Identifying something simple in the environment, like junk food, as having a major impact on developing dementia is wonderful to imagine. If true, we could markedly reduce our risk by committing to a lifestyle free of soda, pizza, and French fries. But there’s scant support for adhering to a Bloombergian regimen as an easy way to prevent Alzheimer’s disease.
In March, researchers reported intriguing discoveries that may predict who will go on to develop Alzheimer’s.8 Scientists from Harvard Medical School and Rush University published in Nature findings about a protein termed REST, found in memory regions like the hippocampus and cortex. In patients with mild cognitive impairment or with Alzheimer’s disease, REST was lost. It appears that the protein can potently protect neurons from the toxicity of beta-amyloid as well as the oxidative stress seen in inflammation. There was a correlation between sustaining levels of REST and preservation of cognition. The researchers proposed that this unique protein may help distinguish between those who will enjoy neural integrity and those suffering degeneration as we age.
Memory can be impaired not only by trauma or by misshapen proteins, but by drugs. The sleeping pill Halcion is notorious for causing short-term amnesia. But in David MacLean’s case, described in The Answer to the Riddle Is Me, it is not immediately clear which drug among the many he took was the cause of his disorientation. He collapsed at a train station while traveling in India:
I was standing when I came to. Not lying down. And it wasn’t a gradual waking process. It was darkness darkness darkness, then snap. Me. Now awake.
…I was in the center of a crowd, half surging for the train, half surging for the exits. I stood still. I had no idea who I was. This fact didn’t panic me at first. I didn’t know enough to panic….
I checked my front pockets for a ticket. Nothing.
Not even a passport.
…Then I realized that I couldn’t even think of what name would have been on a passport if I had one or what foreign country I was currently in. This is when I panicked.
MacLean ultimately asserts that Lariam, a drug prescribed to prevent malaria, is the culprit. He then suspects its potential disruption of memory serves our military as a tool of torture:
In 2008, the DOD [Department of Defense] released a slew of documents pertaining to suspicious suicides that took place at the prison in Guantanamo Bay. Deep within these documents was evidence that beginning in 2002, upon arrival each new inmate was given an initial dose of 1,250 mg of Lariam—a massive dose (five times the prophylactic weekly dose)—before they were tested as to whether or not they were infected with malaria.
He notes that neither Guantánamo Bay nor Cuba has cases of malaria. None of the soldiers or contractors at the base were prescribed drugs to prevent the infection. Professor Mark Denbeaux, director of the Seton Hall Law Center for Policy and Research and legal counsel to Guantánamo detainees, believes that since there is no sound medical reason for administering such a high dose to every detainee, then its psychological side effects were the intended primary goal, “pharmaceutical waterboarding.”
This accusation merits validation by independent medical experts. It is a matter of not only short-term effects from Lariam but persistent debility. MacLean explains that years after taking Lariam,
I am still afraid of lingering chemical instabilities; afraid of what might still be stuck in the wrinkles and folds of my gray matter; afraid of what might get dislodged, disrupting who knows what electrical signals; afraid of where I’ll wake up next.
I finished writing this review on the Saturday night that ushered in the yahrzeit of my mother. The anniversary of her death brings to the fore childhood memories: how she showed me the way to throw a baseball, counseled with clinical certainty that drinking ice water when perspiring was a danger to health, arranged the cereal boxes in alphabetical order in the cupboard. She came from a traditional Jewish family, and one of the first Hebrew prayers she taught me was Modeh Ani, words of gratitude said upon awakening in the morning. The new day is to be greeted as a gift that offers new possibilities.
Physicians often fantasize about which diseases they may develop. In middle age, the shadow of a heart attack colored my thoughts, as many males on my father’s side had suffered one in their fifties. Now, into my sixties, it is impossible not to wonder whether my life ultimately will be marked by a malady where memory struggles to speak. The numbers certainly point in that direction for all of us who are enjoying greater longevity.
If that proves to be the case, I seek some comfort in the fact that remote memories from childhood usually fade last. Those traditional words of gratitude are deeply imprinted, tightly woven in synapses. I hope they resist yielding, so that upon awakening, I still sense possibility.
This Issue
May 22, 2014
The Phony War?
Elizabeth Warren’s Moment
-
1
Suzanne Corkin, “What’s New with the Amnesic Patient H.M.?,” Nature Reviews Neuroscience, Vol. 3, No. 2 (February 2002). ↩
-
2
David M. Bannerman et al., “Hippocampal Synaptic Plasticity, Spatial Memory and Anxiety,” Nature Reviews Neuroscience, Vol. 15, No. 3 (March 2014). ↩
-
3
See Kevin S. LaBar and Roberto Cabeza, “Cognitive Neuroscience of Emotional Memory,” Nature Reviews Neuroscience, Vol. 7, No. 1 (January 2006). ↩
-
4
Susanne Diekelmann and Jan Born, “The Memory Function of Sleep,” Nature Reviews Neuroscience, Vol. 11, No. 2 (February 2010). ↩
-
5
Bryan D. James et al., “Contribution of Alzheimer Disease to Mortality in the United States,” Neurology, Vol. 82, No. 12 (March 25, 2014). ↩
-
6
Jerome Groopman, “Before Night Falls: Alzheimer’s Researchers Seek a New Approach,” The New Yorker, June 24, 2013. ↩
-
7
Fernanda G. De Felice, “Alzheimer’s Disease and Insulin Resistance: Translating Basic Science into Clinical Applications,” Journal of Clinical Investigation, Vol. 123, No. 2 (February 2013). ↩
-
8
Tao Lu et al., “REST and Stress Resistance in Ageing and Alzheimer’s Disease,” Nature, Vol. 507, No. 7493 (March 27, 2014). ↩