When David Shenk set out to write his intelligent and unusually circumspect book The Forgetting, he had, he said, two ambitions: to write a “biography” of Alzheimer’s disease, and to chronicle the race for its cure. A biography of a disease is a strange nomenclature. It suggests, at the start, that Alzheimer’s has a life of its own, one that is distinct from its victims’. Alzheimer’s doesn’t have its own life, except in this: it is animated by fear. A nationwide poll conducted this spring for the Alzheimer’s Association by Peter D. Hart Research Associates found 95 percent of all respondents saying that Alzheimer’s was a “serious problem facing the nation,” and well more than half—64 percent—of those between 35 and 49 years of age reporting that they were concerned about getting the disease themselves. Four million Americans already have Alzheimer’s, a number that is expected to grow to fourteen million by midcentury. As Gary Small, the director of UCLA’s Center on Aging, says in his bullish manual for beating the odds, The Memory Bible: An Innovative Strategy for Keeping Your Brain Young, “we are all one day closer to Alzheimer’s disease.”
By the same logic, then, we are all one day closer to the cure for Alzheimer’s, too. “Ten years to a cure,” a Japanese researcher said to David Shenk in March 1999 at the biannual “Molecular Mechanisms in Alzheimer’s Disease” conference. He, like other researchers Shenk encountered there, was “giddy” at the prospect. Giddiest of all, it seems, was Ivan Lieberburg, the head of research and development for Elan Pharmaceuticals. “We’re really on the threshold of a new age,” Shenk reports him saying. “I think we’re coming very close to the goal line now….”
When Lieberburg said this, it had been nearly a century since a German physician, Alois Alzheimer, first admitted a disoriented, volatile, yet seemingly healthy, fifty-one-year-old woman to his clinic. Unable to remember her own name, she nonetheless accurately described her condition. “I have lost myself,” she told the doctor.
Over the next four and a half years the woman continued to decline, losing the ability to speak, to feed herself, to walk, or to know her own incapacity. Alzheimer was at a loss to diagnose her condition, which did not fit any known model. It was only when she died, and he was able to view slides of her brain, that the doctor found what appeared to be the cause of her premature senility. As Shenk describes it,
…At a magnification of several hundred times, he finally saw her disease.
It looked like measles, or chicken pox, of the brain. The cortex was speckled with crusty brown clumps—plaques—too many to count. They varied in size, shape, and texture and seemed to be a hodgepodge of granules and short, crooked threads, as if they were sticky magnets for microscopic trash.
And that wasn’t all:
In the second and third layers of the cortex, nearly a third of the neurons had been obliterated internally, overrun with what Alzheimer called “a tangled bundle of fibrils”—weedy, menacing strands of rope bundled densely together.
Plaques and tangles—these have, ever since, defined the disease that bears Alzheimer’s name. They are a prominent feature of an Alzheimer’s brain. Still, it remains unknown which phenomenon—if either—causes the neurons to die and the brain to shrink and the body to revert to an autonomic state, and then to die. It is not known, in other words, if plaques or tangles or both cause Alzheimer’s or if they are merely the disease’s signature, left behind in the neural detritus.
Like the majority of Alzheimer’s researchers, the scientists at Elan Pharmaceuticals were guessing the answer was plaques. One of them, Dale Schenk—no relation to David Shenk—had a novel, and many said “simplistic,” idea: vaccinate against them. Since the main component of plaque is a protein called beta-amyloid, which is foreign to the human body, Dale Schenk reasoned that injecting patients with a small amount of it might produce enough antibodies to tag and remove the beta-amyloid in the brain, in the same way that injecting a small amount of a weakened live virus like, say, polio stimulates the immune system to make antibodies to that virus. Schenk further reasoned that since the brain’s natural defense system, the barrier that keeps blood from flooding the brain, was not perfect, and a small number of unwanted particles were always crossing the threshold, injecting beta-amyloid into the bloodstream would result, eventually, in a certain number of beta-amyloid antibodies entering the brain. As David Shenk writes, “[Dale] Schenk’s epiphany was that a body constantly manufacturing its own supply of beta-amyloid antibody would produce so much of it that three parts per thousand would be plenty” to breach the barrier.
Advertisement
In 2000, not long after he baldly hinted that the game was almost over, Ivan Lieberburg went public with the news that Dale Schenk’s hunch had been right. Beta-amyloid antibodies had successfully removed plaques in mice. These were no ordinary mice; ordinary mice do not get plaques and tangles. Ordinary mice do not get Alzheimer’s. Instead, these were transgenic mice that had been genetically altered to grow plaques. What Schenk’s experiments showed was that after vaccination, those plaques cleared up. According to David Shenk,
The injected beta-amyloid was prompting the immune systems to produce targeted antibodies, a small portion of which were crossing the blood-brain barrier and binding directly with beta-amyloid in the brain. Then the offending substances were effortlessly being cleared away as cellular trash.
Dale Schenk and others were able to replicate these results with guinea pigs, rabbits, and monkeys. Further confirmation came from researchers at the University of South Florida. Their mice not only got better, they apparently got “smarter.” Rid of plaque, they were able to negotiate mazes that had stumped them before. “They were normal now, apparently,” Shenk writes in The Forgetting. “For these humanized mice, at least, Alzheimer’s disease was now preventable.”
When Elan Pharmaceuticals announced the preliminary success of the Alzheimer’s vaccine, it was, understandably, big news. The wire services picked it up and sent it around the world; CNN, the BBC, and Time, among others, followed suit. Their reports noted not only that Schenk’s experiment had shown success in the animal models, but that in further trials the beta-amyloid vaccine had proved safe for humans. This did not mean it worked, only that the vaccine was safe enough to test it further to determine its efficacy.
It is at this hopeful moment in the Alzheimer’s story that The Forgetting ends, with the race still on but close enough to being over for David Shenk to reflect, somewhat wistfully, on the meaning of the disease, and what he has come to see as its essential capacity to humanize us:
Through the Alzheimer’s prism, we can experience life’s constituent parts and understand better its resonances and quirks. And as the disease relentlessly progresses toward the final dimming of the sufferer, it forces us to experience death in a way it is rarely otherwise experienced. What is usually a quick flicker we see in super slow motion, over years. It is more painful than many people can even imagine, but it is also perhaps the most poignant of all reminders of why and how human life is so extraordinary. It is our best lens on the meaning of loss.
If that was true then, it remains true. This January, two years after the promise of the beta-amyloid vaccine was broadcast worldwide, and less than six months after The Forgetting was published, Elan Pharmaceuticals had another announcement to make. This one was offered quietly, without fanfare, on its Web site: inexplicably, and without warning, four people participating in the Phase II efficacy trials had developed encephalitis. No one could say why. A month later, in February 2002, eleven more participants out of about three hundred were stricken by a similar brain inflammation. “We never saw a hint of this,” Ivan Lieberburg told a reporter from The Washington Post. “It came as a total shock to Elan.” In March the company permanently halted its trials of the beta-amyloid vaccine.1
In the face of drug failures like Elan’s, as well as the dearth of reliable medical interventions, and in the light of life spans that are challenging the accuracy of actuarial charts, and a generation that can expect to see increasing numbers of its fellows fall victim to Alzheimer’s—see them, pay for them, become them—a literature on popular neurology is burgeoning. These are books written for the affected, a readership that includes—because this disease moves so slowly and insidiously—the potentially affected, which is to say, many of us. They are cultural markers, not only of a particular moment in medical history, but of a growing collective dis-ease.
Typically, and perhaps inevitably, an anxious didacticism connects these books to one another; they consciously play to fear by trading on hope. Even Lawrence Whalley’s straightforward and mostly uninflected dissertation, The Aging Brain, is implicated. A readable academic volume that synthesizes current research to map the changing physiology of the human brain as it gets older, The Aging Brain is offered not only on intellectual terms, but as a palliative. “…This book draws on the startling advances in molecular biological research and computer technology to counter the widespread pessimism about what the future holds in store for us,” Whalley writes in the preface. “These new ideas hold out the possibility of transforming life in old age by preventing or even reversing the damage to brain cells implicated in mental decline.”
Advertisement
In reality, the text of The Aging Brain is more guarded than that. Whalley, who was part of the team that, in the 1980s, discovered a connection between chromosome 21 and early-onset Alzheimer’s disease, is more prone to pose questions than to draw conclusions from the research he reviews. And he is unwilling to interpret the research prescriptively. A discussion on the effect on neurodegeneration of free radicals—extremely reactive chemical compounds, which are naturally produced by the body and have been linked to Alzheimer’s as well as cancer and heart disease—does not lead to the suggestion that readers start swallowing high doses of vitamin E and other antioxidants, but rather to a measured consideration of whether oxidation is a cause or an effect of neuronal damage, and to the suggestion that beta-amyloids themselves may be the culprit, causing free radicals to develop in the bloodstream. “Further study of the neurotoxic activity of beta-amyloid may point to therapeutic strategies (such as vitamin E supplementation of the diet) aimed at…reducing the neurotoxic effects” is as far as he’ll take it.
In another section, Whalley’s consideration of the brain’s essential “plasticity”—its ability to make new pathways and redirect itself, which may be crucial to overcoming certain kinds of brain damage—leads him to this restrained reflection:
There is a well-founded suspicion by researchers that in response to aging some brain functions are more capable than others of this sort of reorganization…. The exciting part of research in this area is the prospect of discovering the sources of these differences. If they prove to have a biological explanation (and many suspect they will), then we may be close to discovering how to retain our mental abilities as we age.
Contrast this with Dr. Gary Small’s exhortation in The Memory Bible: “It is never too late or too early to start beating the brain-aging game.” (Cancer has its war metaphors; dementia is more sporting.) Small’s winning strategy includes getting enough sleep (the brain needs sleep to solidify memory), minimizing stress (stress induces the body to produce cortisol, which interferes with, and can block, memory), eating lots of berries and tomatoes (good sources, among others, of antioxidants), avoiding bad fats (“it is never too early to begin a low-fat diet to keep our brains young and stave off Alzheimer’s disease”), and exercising regularly (more oxygen to the brain, better metabolism of sugars). Most importantly, Small champions a program of mental aerobics—learning a foreign language or doing word or math puzzles or taking up a hobby. These, he suggests, will enable the reader to take advantage of the brain’s plasticity:
The information in our brains is passed through billions of dendrites, or extensions of brain cells, similar to branches of a tree, which grow smaller as they extend outward. Without use, our dendrites can shrink or atrophy; but when we exercise them in new and creative ways, their connections remain active as they pass new information along. And, remarkably, new dendrites can be created even after old ones die.
Evidence shows we can “work out” our dendrites and extend their branches in many ways. Even routine daily activities like lacing a shoe or rinsing dishes can be a trip to the gym for those little guys.
Though your own “little guys” may be a little put off by the doctor’s jocular tone, it’s important to acknowledge that his advice emanates from real science. Positive Emission Tomography (PET) scans have shown greater brain activity when people are learning something new, and longitudinal studies, most famously David Snowden’s fifteen-year investigation of more than seven hundred nuns, suggest that the most engaged minds are least likely to develop Alzheimer’s disease. It is well known that the brain—parts of it—stops working when not used. Stretching the brain—to continue the athletic metaphor—creates neuronal pathways. These pathways appear to become alternate routes when neurons die off in middle and old age.
John Ratey, a professor of psychiatry at Harvard Medical School, takes an approach similar to Gary Small’s. His peripatetic User’s Guide to the Brain starts from the premise that the value of an encyclopedic book like his is primarily utilitarian. “Once we understand how the brain develops,” he writes, “we can train our brains for health, vibrancy, and longevity.” The unsubtle subtext here, as in The Memory Bible and, to a lesser extent, in The Aging Brain, is that any of us—all of us—can avoid our statistical fate, that it is in our power to escape dementia. Indeed, this power is possessed by our very own brains.
“In a system as complex as our brain, it really is up to us,” Ratey says,
and this is why it’s so crucial that we learn about our brains. We do have free will, in a sense, for everything we do affects everything that follows, and the brain develops in a largely unpredictable way. Genetics are important but not determinative, and the kinds of exercise, sleep, diet, friends, and activities we choose…have perhaps equal power to change our lives.
Recognizing, perhaps, our generalized indifference to exercising what Ratey calls “free will,” researchers have spent the past two decades searching for the genetic bases of the disease in an effort to find a medical cure. In what are the most technically challenging and most suspenseful sections of his book, Lawrence Whalley recounts the numerous, overlapping attempts to parse the genetic etiology of the disease. This includes his own research, which contributed to finding a link between Down’s Syndrome and Alzheimer’s on the tail of chromosome 21. Since everyone with Down’s Syndrome has either an extra copy of chromosome 21 or an extra copy of its tail appended to a different chromosome, and since almost everyone with Down’s Syndrome eventually gets Alzheimer’s, the assumption was that there was something to be learned about Alzheimer’s from that small segment of chromosome 21. As Whalley tells the story, molecular geneticists then set out to compile a genetic library of the tail, seeking out, in particular, families with multiple cases of Alzheimer’s. Meanwhile, other researchers, in other labs, were attempting to sequence the beta-amyloid protein:
Careful screening of the gene library extracted from a human cortex found a stretch of DNA that exactly matched the amyloid sequence. This was part of a gene coding for a protein made up of about 695 amino acids, now called “amyloid precursor protein,” or APP…. The next step was no surprise at all: the gene for APP is on chromosome 21.
This led to the discovery that a small number of early-onset Alzheimer’s cases are caused by an error in the structure of APP. Further research showed that other early-onset cases were triggered by mutations of two genes on chromosomes 1 and 14.
Early-onset Alzheimer’s accounts for about 10 percent of the Alzheimer’s population. More commonly, the disease appears after age sixty-five and the number of cases doubles every five years after that. These are the people for whom Alzheimer’s was once thought to be a “normal” expression of aging. And while no one doubts the correlation between age and Alzheimer’s, genetic factors are salient for this group, too. A variant of a gene that makes a protein that transports fat and cholesterol through the body, APOE4 —which appears in 22 percent of the population—seems to increase the risk of Alzheimer’s disease in old people by 40 percent, according to Whalley. How, or why, is as yet unknown. One hypothesis is that it acts as a “molecular chaperone,” escorting beta-amyloid through the brain. Another is that it may compromise the brain’s ability to form new synapses.
It is now possible to screen for APOE4 , to identify people predisposed—though not necessarily fated—to Alzheimer’s. The value of that, Gary Small argues, is to get those people started on a regimen of brain exercises, physical exercise, and a low-fat diet. (He cites a study that showed that people with APOE4 who limited their fat intake “had a strikingly lower risk for developing Alzheimer’s disease.”) Starting these lifestyle changes early, he suggests, may be a way to elude, if not divert, what may appear to be the inevitable. However, because the presence of the gene does not necessarily predict the disease, and because recording its presence in one’s medical record flags issues of medical confidentiality, the National Institute on Aging and the Alzheimer’s Association are both on record as opposing the use of genetic screening to identify people at risk for the disease. For the time being, APOE4 screening is done primarily diagnostically, when Alzheimer’s is strongly suggested. (So far, a conclusive diagnosis can only be made at death, when the brain can be autopsied.)2 It is also used by researchers like Gary Small.
According to researchers, an ineluctable, and very public, predictor for Alzheimer’s disease is one’s level of educational achievement. This holds true in large-scale epidemiological studies like David Snowdon’s nuns’ study, as well as in the work reported by Whalley, Ratey, and Small. So far, no one can say why this is, or how it works; it is conventional wisdom in search of an explanation. Writing of his own examination of a group of apparently healthy young people at the UCLA Memory Clinic, Gary Small and his team found that
when we looked at the effect of higher education added to the effect of the Alzheimer’s APOE4 genetic risk,…as expected,…the young adults with the greatest brain activity had completed college and did not have the APOE4 gene. It is interesting to note, however, that the influence of a college education on a person’s brain activity reserve was even more powerful than that of the APOE4 risk gene…. As yet, there is no conclusive evidence on the mechanism by which education protects brain cells.
It may be that the relationship between higher education and Alzheimer’s is more descriptive than predictive. Certainly, as both Whalley and Small point out, access to education may be the consequence of other advantages that themselves affect health in general and brain development in particular, like good nutrition or wealth. Or it may be that those who choose to pursue higher education are those that have been identified early on as possessing more nimble brains, brains that are already poised, even at an early age, to avoid dementia. Both David Snowdon and Gary Small report that writing samples taken from people in their twenties are also good predictors of Alzheimer’s later in life: the more complicated the sentence structure, the less likelihood of dementia forty and fifty years out. It remains to be seen if, in this country, with an ever-increasing percentage of young people going to college, this correlation holds.
Statistical exceptions do not, typically, prove anything, though often they make good stories. This, ultimately, is the value of David Shenk’s book The Forgetting. Rather than being a biography of Alzheimer’s disease itself, it traces the course of the disease in a number of prominent thinkers and artists, including Ralph Waldo Emerson, Jonathan Swift, and Willem de Kooning. (Of these, only de Kooning’s is a certain case. The others died before Dr. Alzheimer’s disease was “discovered.” David Shenk makes his own diagnosis, based on the historical record.) Each had led a life of intellectual engagement. Indeed, each was mentally active up to the point his intelligence deserted him. (In a moment of rare, and perhaps unprecedented, perspicacity for someone with Alzheimer’s, Swift left this world with the words “I am a fool.”) De Kooning’s case is interesting for the questions it raises about art and intention: What is the value of work created when the mind is riddled with plaques and tangles? But it is Emerson’s story that is most arresting. “We estimate a man by how much he remembers,” Emerson wrote in 1857 in his essay “Memory.” By 1881 he could barely write his own signature, and once he had, could not remember having done so.
Emerson’s decline, so striking to those around him, was, according to his son Edward, unnoticed by the writer himself. This ultimate forgetting, the forgetting of one’s self, is sometimes offered as the sole consolation of Alzheimer’s: the person afflicted is unaware of what is lost. “He suffered very little,” Edward Emerson wrote of his father’s last years.
But how much consolation is that, really? The answer is written on every page of Thomas DeBaggio’s devastating memoir, Losing My Mind. DeBaggio, who made his living as an urban gardener in Washington, D.C., and as a writer, was diagnosed with early-onset Alzheimer’s in 1999, at the age of fifty-seven. An otherwise healthy and physically active man, the author of three books on gardening, a man with a history of political activism behind him and a close-knit family in his midst—none of this was sufficient to override what he takes to be his bad genetic luck:
I get angry…when I hear someone talk about this disease as if it were brought on by improper diet or behavior…. You can do all the healthy stuff touted as a way to extend your life, and you can believe in the 200-year-old human, but do not forget you had parents, men and women who were the results of centuries of genetic swapping…. Although it feels light, every morning you wake up with the weight of your genetic history. It is not your fault you have a battered gene that will kill you, but it is your burden now. Smugness in the pursuit of health is a risky attitude.
There is not a moment of smugness in Losing My Mind. Smugness, like other sureties of self, is no longer available to a mind so full of doubt and silences. (“I have a clear sense of history,” DeBaggio writes. “I just don’t know whether it’s mine.”) The words for things go, and with them a fixed sense of boundaries, and so of place. Long-term memories remain, and in the disjointed, associative ways that we tend to recall them, DeBaggio pieces his own memories together, in no obvious order, to give his life story by both telling (the anecdotes) and showing (their randomness). One is told of his excruciating challenge to compose the sentences and paragraphs in this book, yet does not feel it. The writing is fluent. And remarkably, however hard it is for him to write as he does—however long it takes him to write “Alzheimer’s has taught me it is wise to look in the same place many times for the thing you desire,” or “Lives coast on memory”—the words he does choose are lit with intelligence and the longing for intelligence and for the free will it allows. They illuminate a dark and expanding universe.
Nine months into it, and DeBaggio can carry this torch no further. He resides more in the gaps between words than in language itself. He must quit the book. “I am on the cusp of a new world, a place I will be unable to describe,” he writes at the end. “It is the last hidden place, and marked with a headstone…. It is lonely here waiting for memory to stop and I am afraid and tired.” The silence of the last page, the writer’s silence, is profound.
The competitive engine of scientific research is driven by obsolescence. Soon enough the breakthroughs and protocols recorded by Lawrence Whalley and John Ratey and Gary Small will be supplanted by others, and these books, too, will be replaced by other, more current ones. In the absence of a pharmaceutical or medical cure, some of these new books, no doubt, will be meant to assuage the fears that Alzheimer’s disease evokes. Some may even succeed. Meanwhile, Losing My Mind will not calm anyone’s fears. It is for that very reason—for its base honesty, for its awful beauty—that it won’t go out of date.
This Issue
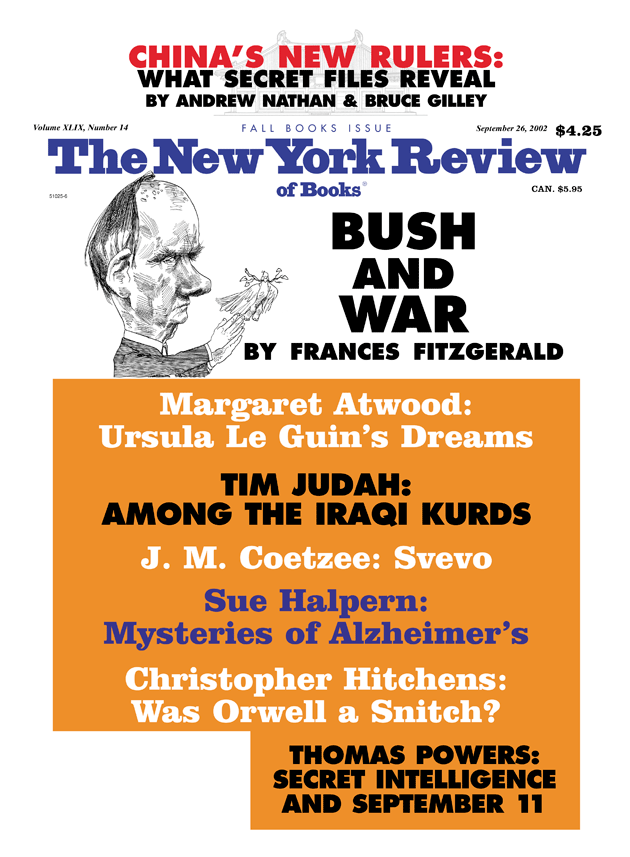
September 26, 2002
-
1
The company continues to pursue an immunological approach to treating Alzheimer’s, and has other Alzheimer’s drugs in its pipeline. ↩
-
2
In a postscript to The Memory Bible, Dr. Small reports that members of his team had just “discovered an innovative method to view the Alzheimer’s amyloid plaques and tangles directly as they accrue in the brains of living people” by injecting patients with compounds that highlight plaques and tangles and then viewing them using PET scans. ↩