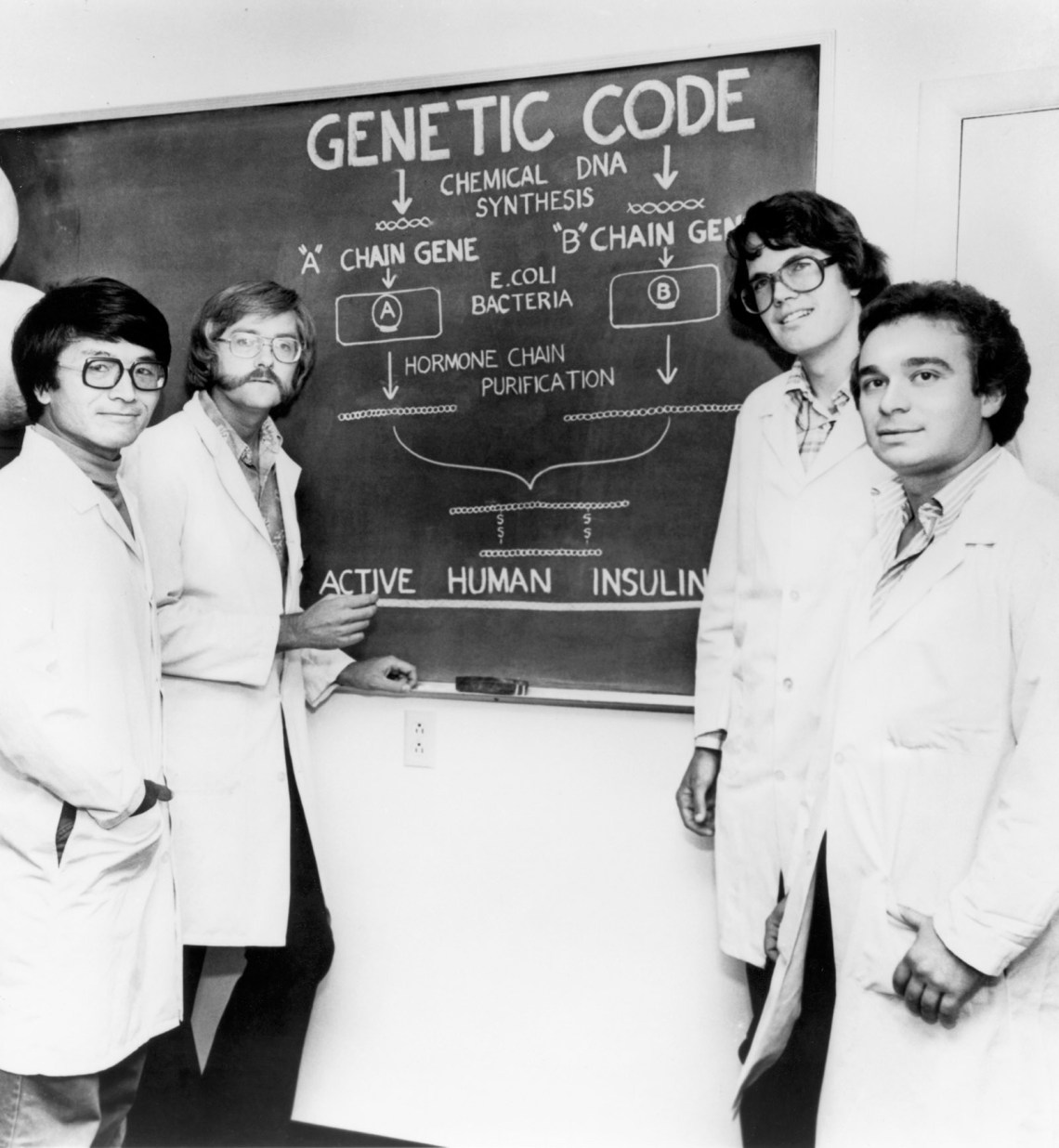
On April 9 of this year, The New York Times featured an obituary for Arthur D. Riggs, a scientist likely unknown to most readers. Riggs’s career was largely spent at the City of Hope National Medical Center in Duarte, California, where he discovered how to use recombinant DNA technology—which brings together genetic sequences from multiple sources—to convert bacteria into factories that produce hormones for clinical use. Among his notable successes was the creation of artificial human insulin. “We chose insulin because it looked doable, and there was a need,” Riggs recalled in an interview last year. “At the time, diabetics were being treated with cow insulin because there was no source of human insulin. And cow insulin resulted in a high rate of allergic reactions.”
Hormones regulate our growth and development as well as metabolism. They may act locally on the tissue that makes them, on nearby tissues, or on distant tissues after entering the bloodstream. When we’re healthy, hormone production is controlled through feedback loops in the body, which prevents either a deficiency or an excess. The disruption of these loops can lead to disease.
Insulin is made in the pancreas and secreted into the bloodstream to promote the absorption of glucose by various tissues, which use it immediately for energy or convert the glucose to glycogen (for short-term storage) or fat (for long-term storage). Insufficient insulin or bodily resistance to it causes high levels of glucose to remain in the blood, a condition formally known as diabetes mellitus. It’s believed that more than 400 million people worldwide suffer from diabetes, which can lead to blindness, nerve damage, tissue necrosis necessitating amputation, kidney failure, and stroke. Every year about four million people die from complications of the disease.
The race to produce human insulin started in the mid-1970s. Riggs and his team at City of Hope partnered with scientists at the biotech company Genentech, which had just been founded. They first attempted to synthesize somatostatin—a hormone about one tenth the size of insulin—but as soon as the bacteria produced the hormone, it fell apart. Riggs’s seminal insight was to link it to a larger protein molecule while still in the bacteria to stabilize it, and only later separate the two. Within a year of conquering somatostatin in 1977, Riggs’s group did the same with human insulin. In 1982 a commercial product, Humulin, was approved by the Food and Drug Administration.
“The discovery made Genentech, and Dr. Riggs, rich,” the Times obituary noted. “But unlike many of his fellow biotech pioneers, he declined the opportunity to make even more money working in the for-profit sector; he was under contract to Genentech, but after that arrangement ended in 1984, he returned to City of Hope full time.” For fifty years he lived in the same modest house. Last year, when he announced a $100 million donation to City of Hope, it was revealed that he had already given $210 million to the hospital anonymously.
Perhaps Riggs’s humble origins shaped his values. He was born in 1939 in Modesto, California. His family lost their farm in the Depression, and his father, who had only an eighth-grade education, moved them to San Bernardino, where he built and operated a trailer park. Riggs’s mother, a nurse, encouraged her son’s interest in science, buying him a chemistry set and ensconcing him in the library. He didn’t feel the need to seek the spotlight with his philanthropy. Gratification came from improving the lives of people through science.
Riggs is one of the many researchers discussed in Insulin—The Crooked Timber, Kersten Hall’s comprehensive account of the modern medical history of the hormone, which was first isolated in 1921. Originally trained as a molecular biologist, Hall now teaches the history of science at Leeds University. He has a personal stake in the story. During “middle age,” he writes, he began to feel lethargic and irritable, then rapidly lost weight and developed “raging thirst and a ravenous craving for sugar”:
A series of blood tests at the hospital confirmed my hunch. There was so much sugar in my blood it was if it had turned to treacle. Poisonous compounds called ketones were raging through my system which, if untreated, would acidify my blood and eventually put me potentially into a permanent coma. My body was in a state of metabolic meltdown—brought on by the onset of diabetes.
There are two forms of diabetes. In type 1 diabetes, the immune system destroys beta cells, which are found in the pancreas and synthesize and secrete insulin. In type 2 diabetes, beta cells still produce insulin, but its effectiveness is compromised. Type 1 diabetes used to be called “juvenile” diabetes and type 2 “adult-onset” diabetes, though it’s now known that the former does not only appear in childhood, while young people can develop the latter.
Advertisement
Hall assumed that, as an adult, he must have type 2, “the one which, were I to eat slightly less, drink slightly less, and run a bit more, might have some chance of being brought under control.” But he was mistaken. It was type 1: “From now on, insulin would be my constant companion—the biochemical crutch on which I would need to lean.” While patients with type 1 and type 2 diabetes both are at risk for serious health complications, type 1 diabetes can be especially hard to control without constant vigilance. Hall quotes a patient who compares it to living with a tiger: “If you look after it, and never turn your back on it, you can live with a tiger. If you neglect it, it will pounce on you and rip you to shreds.”1 Little more is said about his experience with the disease.
Although Hall structures his narrative as a series of biographies of researchers, he rejects the view of scientific progress as linear, without detours and blind alleys:
Alongside ignorance of the history of science, the particular way in which it is remembered can also be problematic. It is tempting to lay the blame for this on Sir Isaac Newton…. Newton famously said that “If I have seen further it is by standing on the shoulders of Giants.” …It conjures up an image that scientific progress is achieved by a succession of either lone geniuses or unsung pioneers far ahead of their time, whose work marks out a smooth, steady triumphant ascent to the lofty pinnacles of present-day knowledge.
I concur with Hall that “the real workings of science” are better captured by Immanuel Kant, who gives this book its subtitle: “Out of the crooked timber of humanity, no straight thing was ever made.”2 In Insulin, Hall does not present
a tale of bold, lone geniuses or saints who set to work on improving the lot of humanity. Instead, it is a story of monstrous egos, toxic insecurities, and bitter career rivalry that at times resembles “Game of Thrones” but enacted with lab coats and pipettes, rather than chain mail and poisoned daggers.
While the discovery that diabetes is a malady of the pancreas related to the hormone insulin dates to the modern era, its symptoms have been recognized since antiquity. The Ebers Papyrus, written around 1550 BCE, refers to a therapy “to drive away the too much emptying of urine,” presumably due to excess sugar. The second-century CE physician Aretaeus of Cappadocia termed this condition “diabetes,” from an ancient Greek word that means “to siphon” or “to flow.” At the turn of the nineteenth century John Rollo, a Scottish doctor, appended mellitus to “diabetes,” from the Greek and Latin words for honey. He had been anticipated by the Hindu physician Charaka, who in the third century BCE recorded that his patients’ urine tasted sweet and that ants were attracted to what he referred to as Madhumeha, or “urine of honey.” (Diabetics’ excess glucose is excreted through the urine.)
In the nineteenth century the pathologist Paul Langerhans found clusters of cells in the pancreas that resembled small islands; they later were named islets of Langerhans. The Belgian scientist Jean de Meyer postulated that these clusters created a substance he called insuline, from the Latin for island. “The hunt was now on to demonstrate its existence,” Hall writes. “The medical rewards of isolating insulin and then applying it in therapy were boundless, for the current methods of treating diabetes did little more than delay a slow and painful death.”
Unlike Riggs, the Canadian Frederick Banting, who helped discover a breakthrough treatment for diabetes, is likely to be familiar to many readers. But I, for one, was not aware of his team’s contentious backstory, which contrasts sharply with that of Riggs and his cohorts at City of Hope and Genentech. Like Riggs, Banting had grown up on a farm, in rural Ontario. He first enrolled in a course in general arts at Victoria College at the University of Toronto in 1910, but he failed his French exam at the end of the academic year and soon had to abandon the arts to pursue medicine instead. Banting’s signature hypothesis was that the antidiabetic substance in the pancreas “was being destroyed by digestive enzymes,” Hall writes, which frustrated efforts to identify it. If you could isolate the islet cells and protect the insulin from the destructive enzymes, Banting posited, you could successfully extract it.
In 1920 Banting approached John J. R. Macleod, a professor of physiology at the University of Toronto and an authority on carbohydrate metabolism and diabetes, with his hypothesis. Macleod, as the senior clinician-scientist, appropriately offered numerous criticisms about Banting’s initial experiment. Most importantly, it lacked rigorous controls. This is how good science should work: frank challenges to experimental methods are vital to avoid misleading results.
Advertisement
But Banting, insecure and suspicious, took Macleod’s suggestions as personal slights. When, in 1923, the two were awarded the Nobel Prize for their discovery, Banting was enraged that Macleod was included, viewing it as “nothing short of a travesty,” Hall writes. Like the Nobel Committee, Hall sees both as responsible for the discovery and quotes Macleod’s own account of it:
Dr. Banting deserves complete credit; if he had not contributed this idea and undertaken to test it experimentally, the discovery of Insulin would probably not as yet have been made. On the other hand, with the knowledge which he possessed of the methods for attacking such a problem he could certainly not have made such rapid progress without careful guidance and assistance.
Banting’s resentment of the older scientist was misconceived. “But for Macleod,” Hall writes, “Banting may have remained a struggling GP in provincial Ontario and never taken those first steps on the road to the Nobel Prize.”
Further advances in our understanding of insulin were made in the 1940s, when the Cambridge-trained chemists Archer Martin and Richard Synge were recruited by a branch of the British government to decipher the protein composition of wool, an important economic resource for the United Kingdom. Working in a converted stable in West Yorkshire, they developed a method to separate proteins known as partition chromatography. Their methodological breakthrough led to the discovery that all proteins, including those found in wool, are composed of ordered sequences of amino acids. Later, Hall writes, the method was used to show that insulin had a precise chemical structure; it also laid the foundation for modern molecular biology by offering “the first hint at how DNA carries the genetic message,” since DNA codes for the ordered sequence of amino acids. Martin and Synge were awarded the Nobel Prize in Chemistry for their development of partition chromatography in 1952 and, unlike Banting and Macleod, seem to have had an amicable partnership. Hall offers many details about Martin’s eccentric personality: a creative genius who ate only certain foods (never fish, no fruit besides apples), he enjoyed sunbathing nude with his girlfriend on Synge’s balcony, drawing complaints from neighbors and a visit from the local constabulary.
Hall notes that when, in the 1970s, Riggs partnered with the ambitious cloning maven David Goeddel at Genentech to be the first to synthesize human insulin, they faced “vocal protest and opposition from a public and media frightened by this new technology.” Indeed, activists were filled with the delusional belief that modern-day Frankensteins, not lifesaving hormones, would be cloned from recombinant DNA laboratories. Fortunately, this delusion has evaporated, and the technology is widely used to produce not only insulin but humanized growth hormone and follicle-stimulating hormone, as well as clotting proteins to treat hemophilia.
Efforts are underway to replace injected insulin with insulin-producing cells created from human embryonic stem cells, which could then be transplanted into patients. This would allow the body to resume producing its own insulin, and essentially be a cure for type 1 diabetes. Douglas Melton, a developmental biologist at Vertex Pharmaceuticals whose two children have type 1 diabetes, is refining the process in anticipation of clinical trials. A single patient treated this way has had excellent control of his blood glucose levels for more than a year without any insulin injections. The use of sources like discarded embryos from in vitro fertilization treatment, however, could become restricted, depending on Supreme Court rulings and which party controls Congress.
A memorable scene in the Woody Allen movie Annie Hall depicts a Jewish family in Brooklyn sitting around the dinner table fixating on illness—“His wife has diabetes!” “Diabetes! Is that an excuse?” “Old Moskowitz, he had a coronary”—satirically invoking a stereotype of Jews as prone to the malady and dilating on its consequences. But as Arleen Marcia Tuchman convincingly shows in her illuminating book Diabetes: A History of Race and Disease, what the film casts as humor, lampooning supposedly neurotic American Jews, has deep roots in the medical establishment’s dark bigotry concerning the origins of the disorder. And the bigotry directed at Jews was redirected in various ways over the past century, making diabetes a case study in how societal prejudice distorts medical science.
Tuchman notes that Germany at the turn of the twentieth century was the acme of clinical science, and its medical literature termed diabetes Judenkrankheit, or a “Jewish disease.” In 1916 Elliott P. Joslin, the leading diabetes specialist in the US, wrote that “the frequency with which diabetes occurs in the Jewish race is proverbial.” Was this in fact true? “Perhaps,” Tuchman answers. “Jewish immigrants who had fled poverty and hunger in Eastern Europe tended to eat better in their new land, and this may have increased their chances of putting on a lot of weight and thus of developing the disease.” While extreme obesity is a clear major risk factor, she cautions that an ample diet does not necessarily result in diabetes, and most overweight individuals are not diabetic. In addition, diabetes has a strong familial incidence, indicating a genetic predisposition to it.
Indeed, there was a dearth of evidence to support claims connecting Jews and diabetes. Instead, Tuchman writes, physicians “simply repeated what everyone else was saying. And those who did offer up numbers and patterns offered statistics that were often unreliable.” Furthermore, the definition of “Jew” was usually ambiguous. Did it include the Sephardim who originated from Spain and Portugal? Or only Ashkenazi Jews? If the latter, were they the German Ashkenazi, who first arrived in America in the 1830s and were generally wealthy by the end of that century? Or the millions of Eastern European Ashkenazi Jews, primarily from the Russian Empire, who began to arrive in the 1880s and were poor? “It is…impossible to answer the question of whether Jews had a higher rate of the disease,” Tuchman concludes.
But we can explore why, despite the highly ambiguous nature of the data—an ambiguity acknowledged at the time—virtually no one questioned the fundamental link between Jews and diabetes during the first three decades of the [twentieth] century.
It came down to negative stereotypes of the “Hebrew race” as loving “high living” and parties where they “congregate together and have frequent and irregular meals.” William Osler, often called the father of modern medicine, added that Jews had a “neurotic temperament,” which he claimed made them vulnerable to the disease, whether because of, Tuchman writes, “nervous strain, nervous temperament, nervous derangements, nervous tension, or the nerve-shattering aspects of city life.” Haven Emerson, a professor of preventive medicine at Columbia’s College of Physicians and Surgeons and a former commissioner of health for the city of New York, “put the onus on Jews for spreading what he called ‘this great luxury disease.’” Here Tuchman links the characterization to “negative images of the Jew as the embodiment of much that was wrong with modernity.” Even Jewish doctors, who denied racial traits, anticipated the Annie Hall scene as they ascribed unbridled nervousness to Jews, drawing on the Oslerian belief that diabetes and the nervous system were intimately connected. This “labile nervous system” was postulated to be an outgrowth of “the long history of suffering, which the Jewish people have had to endure over thousands of years.”
Blacks were also victims of bigotry on the part of the medical establishment and its understanding of diabetes. First they were believed immune to the disorder, which was deemed a “disease of civilization”; African Americans, Tuchman writes, were stereotyped by prominent American physicians as “dull” and “happy” (when not violent) and thus distinctly “uncivilized.” Poor Blacks were thought not “advanced” enough to suffer from diabetes, and middle-class Blacks supposedly “did not exist.” While Tuchman doesn’t offer statistics on how this belief in “racial immunity” to diabetes affected the care African American patients received, we can presume they suffered as a result of it. Only later in the twentieth century, when data on the malady were derived from epidemiological studies in northern cities, did the medical establishment abandon the bigoted view that Black people were somehow immune to diabetes.
A third group whose relationship to diabetes was distorted by prejudice was the diverse peoples known collectively as Native Americans. In 1962 the geneticist James Neel hypothesized the existence of a “thrifty gene,” which offered an evolutionary explanation for how a negative trait might persist at a high frequency in the human gene pool. Neel posited that a “thrifty genotype” might have helped early humans survive periods of feast and famine by increasing their ability to store fat when sufficient food was available. In the modern era, with ready access to food no longer an issue for most people, this efficient storage of fat fostered disease.
By the late 1970s the thrifty gene, Tuchman writes, “acquired the status of a highly plausible explanation, occasionally referred to as a theory, about why Native Americans had some of the highest rates of diabetes not only in the United States, but also in the world.” She adds, “What often goes unnoticed is that Neel did not offer his hypothesis as a way of explaining high rates of diabetes among Native Americans; in fact, he did not even mention them in his 1962 article.” Rather, he aimed to explain the nearly global distribution of diabetes. While Neel was referring to “all the peoples of the world” in his hypothesis on the origin of diabetes in early humans,
the idea of a close link between thrifty genes and indigenous peoples has persisted until today, despite Neel’s abandonment of his own theory before his death in 1999, and despite the lack of any concrete evidence. A belief in racial difference keeps it alive.
Tuchman points out that while there are high rates of diabetes among the Akimel O’odham (Pima), Cherokee, and several other native populations, there are comparatively low rates among other tribes, such as the Athapascan Indians, Eskimos, and Diné (Navajo). Yet both professional and popular writers continue to assert that whites and Native Americans differ in their “experiences of the disease.”
Tuchman ends her book by emphasizing that, most recently, diabetes has become associated with poverty and class. Appalachia, a predominantly white region, is particularly hard-hit. The rate of diabetes in West Virginia, for example, is 10.2 percent, 3.5 percent above the national average. The recognition that diabetes is disproportionately affecting poor populations highlights how social factors as well as genetic predisposition strongly contribute to its development. That poor whites are afflicted further belies the benighted racial stereotypes that have long characterized the disorder. Since the genetic predispositions are not yet addressed by treatment, there is an opportunity to stem the rising incidence of diabetes by tackling the social factors involved.
Riggs wasn’t interested in reaping money for himself from his success with humanized insulin. But since his discovery, money has become a flashpoint in the story of diabetes and insulin, which now extends from science and bigotry to the perverse realities of drug pricing and patents in the United States. The most common forms of insulin can cost ten times more in America than in any other developed country. The price of insulin has nearly tripled over the last fifteen years, according to research cited by the Endocrine Society in a 2021 statement calling for more affordable options for patients. At the outset of the Covid-19 pandemic, the American Diabetes Association found, one quarter of patients with diabetes reported self-rationing medical supplies to reduce the cost of their treatment.
A single vial of Humalog (insulin lispro, or fast-acting insulin), which cost $21 in 1999, cost $332 in 2019, a price increase of more than 1,500 percent. In contrast, insulin prices in neighboring Canada didn’t budge. Why? Because there’s neither a real free market nor government price controls for insulin in the United States. Rather, there is a presumed oligopoly of three drug companies—Eli Lilly, Novo Nordisk, and Sanofi—that appear to set prices in sync, with a vulnerable population of diabetics forced to pay whatever they charge for a lifesaving treatment. Our arcane patent laws allow for extended protection of insulin products without significant innovations, thereby blocking competition. The middlemen who negotiate with the drug companies, insurers, and pharmacies—so-called benefit managers—are enriched by keeping the prices high at the expense of patients. And the insulin manufacturers have a powerful lobbying arm that has kept Congress from taking action.
The issue may be coming to a head, with the Biden administration’s Federal Trade Commission looking into price fixing and Congress asking the Government Accountability Office to investigate pharmacy benefit managers. Governor Gavin Newsom of California recently announced a $100 million initiative to produce generic insulin at cost for patients in his state; whether drug companies will seek to block this by invoking patent protection, as they have done with privately manufactured generic insulin, remains to be seen. The recently passed Inflation Reduction Act limits the monthly cost of insulin to thirty-five dollars for Medicare patients, but Republicans blocked a provision that would have done the same for privately insured diabetics, who are at grave risk of having to ration their insulin unless a remedy is implemented quickly.
Diabetes is a biological illness, but it should also be understood as sociological, economic, and political. Treatment is incomplete unless each dimension is addressed.
-
1
Type 2 can be managed with medication like metformin, which increases our tissues’ sensitivity to insulin. But for patients with type 1, this is not an option, because the pancreas either doesn’t produce enough insulin or doesn’t make any at all. ↩
-
2
Kant’s phrase was used by Isaiah Berlin as the title for his book on fascism and totalitarianism, The Crooked Timber of Humanity: Chapters in the History of Ideas, first published in 1990. Berlin invoked it, in the words of the critic Nicholas Lezard, to argue against fitting “humanity into a straitjacket of their own design.” ↩