1.
The first reactions of many doctors, researchers, and patients to the report of the Presidential Commission on the Human Immunodeficiency Virus Epidemic by retired Admiral James D. Watkins, Chairman, were to admire, with some surprise, the humanity and acuity with which he addressed the AIDS epidemic. These qualities are unusual in bureaucratic governmental reports, and especially unexpected in view of the controversies surrounding this commission: its association with the Reagan administration, the lack of experience or the extreme ideology of some of its members, and the resignation of its first director and another early member. A close reading finds Watkins’s report to be even more coherent philosophically, and more critical of the management of the epidemic, than could be seen at first glance, and it finds the AIDS situation more grave than other recent views have held. It says that we are dealing with a serious and widening national and world health emergency, which is increasingly concentrated in disadvantaged groups—poor women, blacks and Hispanics and their infants, the homeless—whence it is bound to spread further. To contain it will require a nearly limitless budget to effect major social reforms.
The report deals with the incidence and prevalence of AIDS, legal and ethical issues the disease raises, “basic research, vaccine and drug development,” the public health system, an “overview of financing,” and more. Each category is discussed separately, followed by a series of recommendations, and perhaps even more interesting, by a list of “Obstacles to Progress.” Here Watkins indicts “lack of strong leadership,” “excessive concern about potential problems with testing programs and reporting systems,” a confusion about AIDS and HIV, “lack of uniform and strong antidiscrimination laws,” and hundreds of other impediments. The FDA is too slow and disorganized, and working conditions there are “below acceptable standards.” Communities may fail to incorporate HIV information in their classrooms because they “still do not believe the HIV epidemic…will ever affect them.” Admiral Watkins makes the useful point that to use the term AIDS at all is to perpetuate an arbitrary and untrue distinction between the currently ill and those who have tested positive to HIV who will become ill.
The report’s recommendations are specific and sometimes astute: increased funding for primate centers to hasten animal research: a requirement that sharing research data and materials be made a condition of receiving grants; even “assertiveness training” to help people avoid being pressured into unsafe sex. The report makes one conscious of the interconnection of all the remedies: testing and reporting procedures cannot be in place without legal protections against discrimination; without epidemiological data, programs cannot be targeted effectively; reasonable safeguards to privacy must be balanced by the real need of some people (sex partners, health workers, victims of sexual assault) to know who is infected.
That overwhelming revisions of deeply held views are needed is discouraging, in view of what we know about the slowness of social change; but the report is encouraging in that it represents a positive and humane federal position—and that is where change has to start.
The Watkins report is terse. One can get background on it from reading an account like Randy Shilts’s And the Band Played On, a recent history of the epidemic from its beginnings to 1985, with an update to 1987—about the time the presidential commission began its work. Shilts’s story unwinds like a horror fiction—long, rich in subplots, the chronology artfully managed to show the inexorable progress of the disease against a backdrop of social and political paralysis. The villains of the story are government and blood-bank officials who lied about the safety of the blood supply or the adequacy of research funds, feuding scientists, and gay leaders who insisted that the crisis was a homophobic fantasy.
Shilts uses the sinister motif of “Patient Zero,” a Canadian airline steward named Gaetan Dugas, who was so designated by epidemiologists because “the odds on whether it could be coincidental that 40 of the first 248 gay men to get [AIDS] might all have had sex with [Dugas] or with men sexually linked to him” were zero. The incidence of certain diseases among this small group of homosexuals (such as Pneumocystis carinii pneumonia and a rare form of cancer, Kaposi’s sarcoma), formerly thought to be acquired in other ways, led doctors to believe that they were now appearing as complications of sexually transmitted diseases. Early notices of Shilts’s book seized on the sensational detail of “Patient Zero” to convey the impression that he is a leading villain of history but for whom AIDS would not be here at all. But of course the virus was around, waiting to happen. Epidemiologists then did not know of the long latency of HIV infection and now think that Dugas could not in fact have spread the disease to most of those who came down with it within months of their connection with him.1
Advertisement
The sympathetic figures in Shilts’s book are puzzled doctors following hunches and frightened people at the Centers for Disease Control (CDC), the federal biomedical and epidemiological facility in Atlanta to which infectious diseases are reported and which releases controlled drugs for their treatment. Most vivid is his picture of the unsuspecting patients themselves, struggling to understand what was happening to them. Many of them, by now, are dead, and Shilts has recorded valuable testimony of their response to a new bewildering and devastating illness. Whereas Gaetan Dugas, according to Shilts, did not give up sex, others, like Bobbi Campbell, upon learning that they had “gay cancer,” began personal campaigns of public information to help others. A great many had the painful task of nursing friends and lovers.
Faced with the need to make a huge and amorphous crisis seem immediate and human, Shilts chose the device of interweaving individual stories with public events and statistics, which does heighten the emotional impact of his book. The defect of the method is that it confines him to the perceptions of his characters, perceptions that were in the early days of the epidemic overwhelmingly embattled, suspicious, and panicked. This limitation deprives the author of a voice of his own in which to contribute to an ongoing national policy debate that is still afflicted by, as Watkins put it in his preliminary report, “obscene” incidents against people who have tested positive to HIV, by religious codes, by confusion of public health with civil rights concerns—a question Watkins addresses in detail—and by continuing medical mysteries. Further, because the high prevalence of AIDS among IV drug users was not fully appreciated during the period covered by Shilts, most of his examples are taken from homosexuals, encouraging the impression that AIDS is mainly a homosexual disease, whereas now there are signs of declining rates of new infection with HIV among homosexual men, while rates of infection among IV drug users are increasing. In San Francisco, for example, the rate of positive HIV antibody tests among black drug users rose from 15 percent in 1985 to 28 percent in the spring of 1988.2
By late 1981 or early 1982, it had begun to be apparent that something, probably a virus, was killing cells involved in the body’s immune response; this allowed infection by microorganisms to which people were normally immune, and produced a variety of diseases of which Kaposi’s sarcoma (a rare malignancy formerly found mainly in elderly Jewish or Italian men) and pneumocystis pneumonia (a protozoan infection of the lungs that occurs only in persons whose immune systems are severely impaired) were only the most common in a long list. Other complications include oral, fungal, and parasitic infections of the brain, severe parasitic infections of the intestines, and a characteristic dementia.
But although agreement was growing that a virus was probably involved, no one understood exactly how it was being spread. Details of fast-track gay life and promiscuity led astonished researchers, in their effort to find something in the lives of homosexuals to explain the apparent infectiousness of diseases not formerly thought infectious, into such theories as that amyl nitrates (“poppers” used to enhance orgasm) caused the disease.
As early as 1981, workers at the CDC concluded that the presence of infection in IV drug users meant that the infectious agent could be transmitted by needles or in blood and blood products entering the bloodstream, as with hepatitis, a disease also common in homosexuals, and they began to be concerned that the blood supply could be contaminated. In 1982, the first case of pneumocystis pneumonia was diagnosed in a hemophiliac, evidently contracted from the blood product concentrate hemophiliacs are given to allow their blood to clot. While this was only one case, and no autopsy was performed to rule out other causes, CDC workers began to watch the blood supply with apprehension.
Shilts chronicles a general lack of cooperation and mutual suspicion among health agencies, health workers, and patients in these early days. Dr Arye Rubinstein, a pediatrician in the Bronx, was unable to convince anyone that infants were contracting the same disease as homosexuals. Colleagues of Dr. Michael Gottlieb, a Los Angeles immunologist, “continued to urge him to get out of AIDS and back into a more ‘legitimate’ area of scientific research.” Shilts has assembled from press reports, nine hundred interviews, public health records, and from documents secured after challenges by the Freedom of Information Act, much evidence suggesting that medical progress was slowed because the disease affected marginal groups, and because it touched on emotional issues surrounding sex and drugs, and other sensitive corollary questions such as those of privacy and legality. Who should be tested for the HIV virus, and what are the rights of a person who tests positive? Such issues became a source of disagreement among the members of the Watkins commission, whose report takes exception to some current administration policies, for instance, the mandatory testing of immigrants.
Advertisement
In the long run, the fact that many of the affected homosexuals were middle-class, intelligent, professional, and organized meant that they possessed at least some resources to combat the spread of the disease. Initially, however, they were confused and polarized. Shilts’s account of resistance among homosexuals to closing bathhouses in San Francisco or giving “safe sex” advice suggests some of the political difficulties that lay in the way of implementing AIDS health measures. As early as 1982, public health officials became convinced that AIDS was being spread by promiscuous sexual practices, but as late as 1985 in San Francisco, the recommendation of public health authorities to close the bathhouses, scenes of much of this activity, was opposed by many gay leaders as an infringement of their newly won sexual and political freedoms, and any educational and publicity measures restricting these freedoms were seen as part of a homophobic conspiracy. Dr. Mervyn Silverman, the health director of San Francisco at the time, mindful of sensitive political realities, was forced to choose between offending a powerful political constituency for its own good, and making the bathhouses an issue that the homosexual community would defend, or risk later charges of irresponsibility and neglect for not having closed them sooner. As it happened he stood accused of both, and the opportunity to use these places to dispense information and cautionary literature was lost.
Frances Fitzgerald, in a detailed account of the bathhouse crisis in Cities on a Hill,3 is more sympathetic than Shilts to the dilemma of the city’s health authorities. She feels that “it would have been very difficult to second-guess any one of the decisions” the San Francisco health director made, and quotes a psychotherapist who followed the reaction of homosexuals and found it not unexpected that they went through “the stages that individuals are said to go through when faced by a life-threatening disease: denial, rage, bargaining, acceptance.” In the early stages of this process, according to Shilts and Fitzgerald, many homosexuals simply blocked efforts to alert others to the dangers of AIDS and derided those, including Shilts, who tried to spread information as the enemies of gay freedom or at least as damaging to business in the Castro area of the city.
Shilts presents, too, an ugly picture of the cupidity and mendacity of the blood banks, those trusted and supposedly watchful guardians of the nation’s health, who were quick to collaborate with groups “organizing to oppose what they called the ‘quarantine of gay blood.’ ” More than a year after it began to be suspected that the virus could be contaminating the blood supply, the major blood-banking institutions (Red Cross, American Association of Blood Banks, and Council of Community Blood Centers) still refused to believe CDC reports of documented cases of AIDS that could be directly traced to contaminated blood, rejected all but cursory screening of blood donors, and, applauded by gay leaders, issued a statement that “direct or indirect questions about a donor’s sexual preference are inappropriate.”4
The secretary of health and human services, Margaret Heckler, as late as 1983 assured the public that US blood was “100 percent safe” and was supported by local officials and the press. Stanford University was one of only a few hospitals in the country where blood was tested for hepatitis B, which, because it was a readily detectable sexually transmitted disease in homosexuals, had proved reliable in predicting donors “at risk” for AIDS. But other Bay Area hospitals did not adopt the practice until nearly a year later, despite mounting numbers of AIDS cases that could be traced to blood transfusions. By 1983, one hundred people, including several elderly grandmothers, a number of infants, and a nun, had been infected with HIV from blood transfusions and later developed AIDS. A screening test for the virus itself did not become available until February of 1985; even then its release date was delayed by suits from gay groups “pending verification of the test’s accuracy and a guarantee that the test labeling would not mark the start of massive…screening of gay men.”5 It has since emerged that the US blood industry continued to supply unscreened blood to foreign countries after the test was available.6
Many of Watkins’s criticisms of the slow federal response to the growing AIDS epidemic are documented by Shilts. There were conflicts between the National Institutes of Health and CDC, feuding scientists, and researchers competing for grant money—the kinds of discord that seem to trouble most hurried, large-scale medical efforts. Shilts charges that the leading virologist, Dr. Robert Gallo of the National Cancer Institute (who is credited with isolating HIV shortly after the French scientist Luc Montagnier did, and with being the first to discover how to grow it in large quantities), jealously guarding his chances at the Nobel prize, refused to share research materials with investigators at the CDC, including a former employee of his own laboratory who went to work there. The Watkins report finds that a lack of standardized research substances still “makes information coming from different experiments difficult to assess,” and it deplores the antiquated facilities and general disorganization among government health agencies, which make it hard to compare results.
Shilts believes that had Gallo, Montagnier, or other virologists turned their attention to finding the virus sooner, much time would have been saved. Certainly when scientists did begin to look for it in earnest, it took only a matter of months to find it. But a huge obstacle to progress in AIDS research, identified by both Watkins and Shilts, was the unwillingness of the Reagan administration, for political and financial reasons, to mobilize federal resources to combat a serious and steadily increasing problem.
The government has recently become more receptive. Congress has appropriated more than $900 million for support in this fiscal year, nearly twice the amount spent in 1987, and the President has requested $1.3 billion for fiscal 1989, but Watkins warns that federal bureaucratic procedures, which have impeded “a timely response” to the epidemic have to be drastically reformed for this to be of much use. He has asked for more than $3 billion in fiscal 1988, and in view of the magnitude of the research and treatment efforts he finds essential, one questions whether even this would be nearly enough to implement the commission’s recommendations.
Shilts’s picture of despair and frustration in the early years of the epidemic among those researchers who sensed what was happening and among the increasing number of victims, is on the whole powerful. Both groups seem to have been largely correct in their impression, common in people who cannot enlist others in a cause they believe in, that few people cared about them. Shilts believes, apparently with reason, that this indifference was in part owing to homophobia. But besides homophobia, one can also see self-interest and muddle, and can as easily conclude that much of the progress that was made may have been because the victims themselves were an intelligent, articulate population with growing political power, instead of, say, poor Haitians, or a troublesome and inaccessible group like IV drug addicts.
In any event by the time some reasonable understanding of AIDS and how it is transmitted had been acquired, hundreds of thousands of persons had already been infected. One particularly important study of the incidence of HIV infection was made at a San Francisco clinic for sexually transmitted diseases, where a group of 6709 homosexual and bisexual men were recruited, beginning in 1978, for a study of hepatitis B. Because their blood samples had been taken routinely and stored, they were available for analysis later on, after the HIV antibody test was developed. It has thus been possible to see how many of the subjects have acquired HIV infection, and when and how many have come down with AIDS. Retrospective blood tests of one group of 283 men who had been vaccinated against hepatitis B show that all but 3 were free of the antibody to HIV in 1978, and that the incidence of new infections rose to a peak of 20.8 percent of new cases in 1982 (fifty-nine cases), and then the rate fell sharply by the end of 1983. In 1986, the rate of new infections was less than I percent.7
This striking decline occurred just when the epidemic was beginning to attract the attention of the general press, outside scientific journals. It would suggest that the disease may have spread in homosexual high-risk groups during the late 1970s and early 1980s until a high percentage of their members were infected. But after 1983, when the HIV virus was isolated and the facts about HIV infection became more widely understood, many homosexuals changed their behavior. The incidence of cases of new HIV infection among male homosexuals is now so low as to suggest that the epidemic may have already run its course in that group—although most of those who are infected have yet to develop AIDS. But among drug addicts, in whom comparable changes in behavior have not so far occurred, evidence of new infections continues to rise.
2.
Much more is now known about the particular biology of HIV and how it causes AIDS than even a short time ago, but information about several key points is still being revised.
AIDS is caused by HIV, a virus that belongs to the family of retroviruses. Retroviruses carry their genetic information in the form of RNA (ribonucleic acid), unlike other viruses, such as influenza, which are composed of DNA (deoxyribonucleic acid), the same substance that forms genes and chromosomes in all living cells. With the aid of a special enzyme, reverse transcriptase, HIV produces a DNA copy of itself and permanently implants its genetic code within the genes of a host cell, making it necessary to kill the cell in order to kill the virus.
Although HIV is only able to infect certain cells, those that bear identifying molecules called receptors on their surface membranes, some of the cells that are infected—the helper T-lymphocytes, circulating monocytes, and tissue macrophages—are particularly important in controlling the immune system and responding to immune challenges. Destruction of the helper T cells produces the immunodeficiency that leads to AIDS, and the monocytes-macrophages become permanent distributors of the virus throughout the body and factories for its replication.
The virus can be introduced into the body of an uninfected person in only three known ways: nonsexually by mixing contaminated blood or blood products with one’s own blood (usually by injection but rarely through broken skin); by the exchanges that occur between an infected mother and baby during pregnancy, birth, or breast feeding; or by sexual intercourse, through the exchange of blood, semen, or vaginal secretions containing the virus. There is no evidence that HIV can be transmitted by inhalation, ingestion, insect bites, casual contact, for instance on dishes, or even the more intimate, nonsexual contact that occurs among family members.
It is clear that anal intercourse is the most hazardous type of sexual activity, especially for the recipient, whether male or female, because during anal penetration the delicate membrane lining the rectum is often torn, allowing the virus access to the bloodstream, and because specialized M cells located in the rectum facilitate entrance of HIV into the body in some way still unknown.
As of July 18, 1988, the CDC reported 67,141 cases of AIDS nationwide among adults. (See the box above.) In addition there were 1,049 cases of AIDS in children, mainly (78 percent) in infants born to mothers with HIV infection or AIDS, and most of the rest from transfusion or blood products received in treatment of hemophilia.
These statistics show distinct changes over the past two years: besides the decreasing percentage of new cases in male homosexuals, and a rising percentage in intravenous drug abusers, the percentage attributable to heterosexual transmission, now 4 percent, has doubled during the last few years. But part of this increase can be explained by a change in the reporting criteria, and the addition to the “heterosexual” category of people born in Haiti and African countries. These were formerly categorized separately because it was initially believed that some special susceptibility or practice, not heterosexual intercourse, accounted for the incidence in these groups. The Watkins report concludes that, in the US, whether or not HIV will spread more widely among heterosexuals, as it expects, depends on whether the behavior of IV drug addicts can change. Right now, heterosexual transmission in the US is largely confined to the sexual partners of bisexual men (18 percent), and, above all (70 percent), to those of IV drug users, and to persons from countries such as Haiti where heterosexual transmission is in fact the dominant means of spread.
AIDS is increasing among blacks and Hispanics in the US. According to the most recent CDC data, whereas blacks make up 11.6 percent and Hispanics 6.5 percent of the population at large, they make up 25 percent and 13 percent of AIDS cases respectively. Among children with AIDS, 56 percent are black and 20 percent Hispanic, and among women 51 percent are black, 20 percent are Hispanic. It is clear that these statistics reflect the high rates of IV drug abuse in these groups, but the CDC notes that the prevalence among blacks and Hispanics is also “disproportionate,” even allowing for the high rate of drug abuse that places them in high-risk groups. A similar disproportion in black and Hispanic cases has long been noted in tuberculosis. The question whether there is an innate susceptibility to tuberculosis among these groups, or whether the increased prevalence is owing to increased exposure, has been studied exhaustively for decades and has never been resolved. At present a black heterosexual IV drug abuser has twenty times the chance of having AIDS than a white in the same category. AIDS is the leading cause of death among all IV drug users. Black and Hispanic prostitutes, too, show a higher rate of infection than white prostitutes, even where IV drug use is not involved.8
Although most of the world’s approximately 100,000 reported cases of AIDS are in the US and Europe, the World Health Organization estimates that there are probably more than twice as many worldwide,9 mostly in Africa, and that anywhere from five to ten million people may already be infected with HIV. (Following past experience, WHO expects more than a million reported cases of AIDS by the early 1990s. These projections, it should be added, are very crude because the statistics of current infection are incomplete.)
But whereas the Western cases have mostly been transmitted homosexually, it is believed that, in Africa, transmission is mainly through heterosexual contact. Because epidemiological work in AIDS in Africa is still frequently inadequate—hindered by lack of money, by local customs, and by politics, in particular the tendency of some African governments to see racism in theories that AIDS started there—no one seems to know exactly what it is that encourages heterosexual transmission in Africa but not here. Western observers have speculated broadly: genital sores, brutality in sexual intercourse, anal intercourse, clitoridectomy, bisexuality, increased promiscuity as a result of overcrowded conditions in the cities and the accompanying breakdown of the family, malnutrition, and generally lowered immune systems. Recent reports from Zaire suggest that the increase in cases has been occurring mainly in cities and that the incidence has remained stable in rural areas where families and the pattern of life are unchanged.10
In reading Shilts’s account, and in following the daily reports of AIDS developments since his book appeared, one has been struck by how regularly each new aspect of the problem is at first resisted on an emotional and superstitious level before reason and responsible action begin. Nowhere are the effects of myth and fear clearer than in the matter of the transmission of HIV in Africa where the elaborate explanations of dark customs and sexual practices just mentioned seem to arise because people are reluctant to face the unpleasant conclusion that AIDS can be spread heterosexually by vaginal intercourse. In fact, sex in Africa is overwhelmingly “penilevaginal,” though promiscuity is important and prostitution plays a larger role than here.11
One wonders if reluctance to believe in heterosexual transmission might also account for the assignment by the CDC of “men reported only to have had heterosexual contact with a prostitute” into the risk category “undetermined” rather than “heterosexual,” though epidemiologists explain that this category is used because the overall rate of infection among prostitutes in the US is low, and because there have been feminist objections to emphasizing the role of women in transmitting HIV. In fact the rate of infection among prostitutes is 57.1 percent in Newark and 18.7 percent in Miami, which does not seem low.
In the absence of foresight, epidemiologists must guess the future of the HIV epidemic from mathematical models of probability constructed from what they do know for certain about the prevalence and behavior of the virus up until now. A given set of statistics can lead to different conclusions depending on the assumptions underlying the model. Thus the future of the HIV epidemic has been viewed in different ways with different conclusions. Looked at from the perspective of the relative inefficiency of most heterosexual transmission, the spread of HIV among heterosexuals would be slower. Another theory is that sexually acquired herpes and other types of genital ulcers, which are common in Africa, would increase the rate of heterosexual spread by facilitating transmission of the virus. One model hypothesizes that the rate might therefore be slower in countries where these ulcers are uncommon. Or, as University of California epidemiologists note, “Heterosexual transmission may become more evident as the epidemic matures.” Watkins says that most present models have the defect that they are based on the classical history of epidemics and there is no reason to assume that AIDS will necessarily follow the classical model, according to which a group would be saturated and the incidence of disease would begin to decline.
Another theory is that “heterosexual transmission could become more evident as the pool of infected women slowly increases. This hypothesis is supported by the changing epidemiology of AIDS in Haiti, where, over time, the primary risk group associated with AIDS shifted from homosexual to heterosexual individuals.”12 This last appears to be the hypothesis the Watkins commission has found most convincing, because it most nearly describes what has actually been happening. But the commission complains that all existing models are “too simple,” based as they are on incomplete data, tenuous assumptions, and statistics that, because they are broken down crudely, largely ignoring age, for example, have a limited value in prediction.
What seems most likely is that HIV has not spread heterosexually at a higher rate in the US because of the social factors (poverty, social class, ethnicity) that confine heterosexual victims and drug users to the same group. The Watkins report proposes a number of measures that could help to slow the spread of AIDS among drug abusers (treatment on demand, expansion of treatment centers, etc.). Some cities have initiated clean-needle programs and distributed educational material about sterilization of needles with bleach or other agents in an attempt to reach the drug-abusing population. The projection of 450,000 cases of AIDS by 1993, a number based on those currently infected with HIV, is likely to be correct, but what happens beyond 1993 will depend on rates of new infection—in other words on preventing transmission now—by reaching drug addicts and modifying their behavior. Unless this vulnerable group can be encouraged to use clean needles, and avails itself of drug treatment programs and whatever AIDS treatment is available—and unless these programs are made available—an ongoing and fatal epidemic will be added to the other burdens of the poor.
3.
As in Africa, no one really knows how many people have HIV infection in the US. Anonymous tests done on blood from umbilical cords in newborn babies produce different results depending on where the specimens are obtained: reports published last fall indicated that one in 476 babies born in Massachusetts showed antibodies to the virus, but one in 125 in the “inner city” hospitals and one in 77 in New York City. In the frequently quoted 1986 Coolfont Report the US Public Health Service estimated between 1 and 1.5 million cases in the US. Although other widely varying estimates have been made, the CDC recently reaffirmed a number between 945,000 and 1,400,000.13 In the hope of arriving at a more precise figure, the CDC wanted to perform HIV tests on blood from 50,000 randomly selected Americans, but when 2250 people were asked whether they would participate in such a study, 31 percent refused, despite assurances of privacy.14 Presumably people did not want to know the results of such a test, or feared that the results would not remain private.
The Watkins report emphasizes that while confidentiality must be protected, it has to be balanced against the urgent need of some people (sexual partners, health workers) to know who is HIV-positive, and that therefore strong civil rights protections must also be in place to safeguard the jobs, housing, etc., of people known to have been infected. Watkins continuously emphasizes, also, that testing HIV-positive, not the presence of AIDS (the ultimate complication of HIV infection), must be the criterion on which health care and civil rights are based, since the condition and future of the HIV-infected are grave no matter how advanced the clinical condition.15
We cannot predict how much time can pass between infection with HIV and testing positive for it. A positive test usually occurs between six weeks and six months of infection, but cases have been reported in which the response was delayed as long as fourteen months,16 and nobody knows for sure how long the latency period can last. Once HIV becomes part of a host cell’s genetic apparatus, it may lie dormant or it may be activated in response to signals that are poorly understood; perhaps such a signal is given when the immune system is set off by “co-factors,” for instance, infection with other microorganisms, like those causing syphilis or hepatitis. Upon replication, new HIV particles are released to infect other cells, and the originally infected helper T cells are killed, steadily decreasing their number and thereby impairing the immune system and setting the stage for the later development of AIDS.
After HIV has entered and implanted itself in the body, the person has HIV infection, which he or she, while not necessarily sick, can transmit to others, but his or her blood tests will remain negative until antibodies are formed, a sign that the immune system has recognized the new invaders. During this period, the victim might unknowingly infect others, or might donate blood that would also escape detection by blood bank tests as they are performed at present. (Watkins advocates that the states adopt uniform criminal penalties for knowingly passing on HIV, although some commission members argued that existing assault laws could serve if applied.) Indeed, HIV infection has been documented in thirteen recipients of blood from seven donors who tested negative for HIV antibodies at the time they gave blood but who later turned positive. Obviously there is now “a remote but real risk of HIV infection in persons who receive blood screened as negative.”17 Newly developed highly sensitive tests of the DNA for the virus itself, not just for antibodies, can eliminate this problem but these are not commercially available to blood banks yet and are probably at least a year away. Studies using this DNA testing technique have found HIV living and reproducing in macrophages without either invading the helper T cells or triggering production of antibodies. No one knows how long this type of latent infection can last or how commonly it occurs, but its implications are ominous.
How many persons with HIV infection, that is, who have tested positive, will develop AIDS is not definitely known, but the picture becomes bleaker with passing time. The longest follow-up study is another sample of the 6709 homosexual or bisexual men, recruited from the San Francisco City Clinic for sexually transmitted diseases. Studies of the entire San Francisco group, including those whose blood tests became positive during the course of the study, indicate that the likelihood of developing a serious complication of HIV infection increases continuously from the time the blood test became positive, and that there is no evidence of a period after which the incidence diminishes—if anything the risk increases after five years. (After three years of testing positive for HIV 5 percent will develop AIDS, but after five years, 15 percent will have it, and after seven years, 30 percent, and so on.)18 Similar results—that more and more HIV victims become ill as time goes on—have been reported from smaller studies of other adults at risk of developing AIDS in which the duration of HIV infection was known. From these data, the CDC estimates a rate of 99 percent occurrence of AIDS among HIV-infected persons, with a mean incubation period of 7.8 years.19 Using these figures the US government now expects there will be 365,000 cases of AIDS in the US by the end of 1992 and 450,000 by 1993.
To date there are no reported cases of recovery from HIV infection. The length of survival depends on the disease that led to the diagnosis as well as on its response to treatment. In addition, there is more and more evidence that drugs, like azidothymidine (AZT), which acts by inhibiting the enzyme that causes HIV to produce a DNA copy of itself, can prolong survival in patients with AIDS.
The original AZT trial was terminated after a few months when those receiving the drug had fewer opportunistic infections and deaths than those receiving a placebo. As soon as AZT was shown to be beneficial, it was made available to the surviving patients who had received the placebo in the original trial, and all have been followed closely for nearly two years. Now, although the disease has progressed and many of the participants have died, the overall average life expectancy among them appears to have been extended from twelve to eighteen months, and many patients continue to do well up to the present.
But AZT also has considerable toxicity. In general, the sicker the patient to begin with, the greater the side-effects of AZT. Only about 50 percent of patients with advanced AIDS are able to tolerate the drug, while less severely ill patients do much better. At San Francisco General Hospital, forty of forty-two patients who had recovered from their first episode of pneumocystis, were able to tolerate AZT for at least six months.
Because of its side-effects, AZT is now being tested in varying doses in HIV carriers without symptoms and in patients with early or mild HIV complications in order to see what minimum dosages might be effective. But because there is such a long latency period in HIV infection before complications occur, results of this test will not be known for years. Seventeen other drugs with anti-HIV activity, such as ribavirin and dideoxycytidine, are being tested alone, and others—interferon alpha and acyclovir—in combination with AZT, but it is far too early to tell what effect they will have. They are likely to prolong life, perhaps substantially, but none is expected to cure HIV.
Another approach to treatment is to repair the immune system damaged by HIV by various “immune-enhancing” methods. Studies are under way with drugs such as interferon alpha (which also can act against the virus itself) and isoprenosine, which may stimulate lymphocytes—the cells important in forming antibodies—within the body, or with the patient’s own cells that have been removed, treated with inter-leukin-II, and then reinjected. Bone marrow transplantation has also been tried a few times. So far none of these approaches to HIV infection has been notably successful, but several new techniques of stimulation of the immune system are currently being investigated.
Since the FDA liberalized its rules in order to hurry tests of new drugs, only one sponsor has applied for permission to do so. The Watkins commission, while critical of the cumbersome approval procedures of the FDA, also cites the numerous other factors that discourage drug development—liability and antitrust laws, tax problems, paperwork—which outweigh the incentives. And Watkins mentions dozens of other unsolved problems, including those attending the development of an HIV vaccine. Studies in Bethesda, Paris, and San Francisco have shown that at least three well-defined strains of HIV exist, and that a completely new retrovirus (HIV-2) has recently been isolated from patients with AIDS in Europe and Africa (and it has also turned up in New Jersey). Obviously, like influenza and some other viruses, the HIV viruses may defy attempts to create a single all-purpose vaccine, and many will be needed. Indeed, all the vaccines tried to date have failed to prevent HIV infection in chimpanzees, the only animal that has been available for testing so far in which the virus will live after innoculation. Chimpanzees do not get AIDS. Despite these failures, vaccine trials have already begun in human beings, but because of legal liability, “undefined” research ethics, and the lack of basic knowledge, Watkins predicts that progress will be slow here too.
4.
The AIDS crisis has posed serious ethical questions, and it is here that the Watkins commission has shown unexpected breadth in its grasp of the problem. Undoubtedly the most contentious issue is mandatory HIV testing (not including the routine screening of blood donations, which everyone agrees must continue). The commission makes the point that epidemiology cannot succeed without legal protection for people who test positive. Like any laboratory test, the HIV-antibody test has a certain percentage of false positives—people who turn out positive when they in fact are not infected—and false negatives. In a large population where the actual prevalence of the virus is low, many people would simply receive the wrong information. The New York Times explains that
if a low-risk group—like blood donors in Peoria, for instance—were screened for AIDS by the Elisa test, with its positive results confirmed by the Western blot test, 89 people out of 100,000 would be labeled as carrying the virus. But the real incidence of AIDS [sic—what is meant is prevalence of HIV] infection among this group probably is 10 per 100,000. The tests would miss one of the ten, catch the other nine and falsely describe 80 other people as carriers of the virus…needlessly devastating dozens of lives for every case of infection detected.20
The federal government has enacted an expensive program of compulsory HIV testing of potential immigrants, which has so far uncovered only six HIV-positive people, and prisoners in federal penitentiaries—people whose “rights” are limited. The armed forces now test recruits and personnel on active duty, the State Department tests foreign service officers and their dependents, and the Peace Corps and Job Corps test all their applicants. But the Watkins commission disputes the value of all testing, urging only mandatory testing of sex offenders, but otherwise supports only voluntary testing in all groups. At the same time, because of the importance of having research data on the prevalence of the disease, the commission has voted to urge that results of all tests be reported to the federal government.
Indeed, besides counseling, it is not clear what can be done with people who test positive, at least until there is evidence that AZT or some other drug could be effective in mitigating the effects of the virus. (South Africa is repatriating people who have tested HIV positive to their countries of origin, and there are rumors that Cuba has interned them.) The federal government a few months ago took an enlightened position, allowing federal employees with AIDS to work as long as they can, making discrimination illegal, preserving confidentiality, and addressing, with counseling if necessary, the fears of other employees, but Watkins goes further in calling for legislation on these points.
In an aside on morality the commission holds that an HIV-positive person has the primary responsibility for notifying his sexual partners and his doctors. All of the members of the Watkins commission did not agree with all details of the preliminary report, for instance, that the intentional transmission of the virus be made a criminal offense. But all agreed to recommend that public health authorities, using information supplied by doctors, be required to notify the sex partners of the HIV-positive if that person will not do so—one of the eight situations where the need to tell someone is deemed to outweigh the individual’s right to confidentiality. The principle that this right does not outweigh another person’s safety—physician, nurse, partner—is hard to disagree with. Doctors are already obliged to report cases of syphilis and tuberculosis to their local health departments and it seems reasonable to do the same with HIV infection. Yet one can see the vast potentiality for loophole and leak that could cause harm to the HIV infected.
The Institute of Medicine of the National Academy of Sciences in a recent report21 points out that “treating HIV infection and AIDS like other reportable diseases helps to dissipate some of the stigma associated with HIV infection, and thus it normalizes the disease.” The arguments for and against mandatory notification of partners center on feasibility, as well as on the question whether this may “discourage individuals from seeking voluntary testing, a cost that does not justify its potential benefits,” as the Institute of Medicine report puts it. Both reports agree that doctors should not have a legal obligation to notify partners—they have already been sued both for notifying and for not notifying.
The Institute of Medicine does not recommend that “mandatory reporting of sero-positive test results with identifiers” (i.e., the names of carriers of the virus) should be required at this time, and it believes such notification programs should be voluntary. Here one wonders how much tracing and notification, especially among high-risk groups, are really possible. In view of all this, the reasoning behind Watkins’s call for firm legal protections of those known to have HIV is particularly important. Even with legal protection, the commission’s wistful exhortations of good will and cooperation reminds us that although “liberty entails a responsibility not to harm or interfere with others, a responsibility to be non-maleficent,” we can’t count on it.
The Watkins report concludes that
a society is judged by how it responds to those in greatest need. A tragedy such as the HIV epidemic brings a society face to face with the core of its established values, and offers an oportunity for the reaffirmation of compassion, justice, and dignity.
It finds encouraging signs that these qualities are not altogether absent here. At the same time, the report confronts, in tones of dawning realization, the woeful inadequacies in present policy, funding, and the state of knowledge of basic human behavior—it notes that information on sexual behavior still comes from Kinsey. The commission calls for huge increases in behavioral as well as biomedical research. One senses in the report a kind of stupefaction, the tone perhaps of an able military administrator seeing for the first time the disorganization and inefficiency of the federal health agencies—for instance, the way prevention programs are budgeted only from year to year. It is dismayed to find that “there are no entitlements for immunization for all children in the United states. There are just year-to-year dollars eroded by inflation.”
The only defect of the report, one could say, is its possibly naive faith in the ability of social science to answer difficult questions of human behavior—questions which as posed by the commission may themselves sometimes be naive: e.g., “why women may choose to get pregnant and bear children even though they know they are infected with HIV and have an approximately 50 percent chance of infecting their child.”
But among its strengths, certainly, is a sophisticated understanding of cause and effect in human nature unusual among doctors, social scientists, and probably also among admirals. Admiral Watkins and his commission understand that drug companies will not develop new drugs without tax incentives and profit; that doctors will not treat with experimental drugs if they are afraid of being sued; that women will not become nurses for low pay and low status; that people without hope of a good life may have little reason to avoid illegal drugs; that people who fear losing jobs and homes will not submit to testing. Therefore, society should address the tax structure, the malpractice laws, the pay and education of nurses, the welfare of the poor, and the system of legal protection for HIV-infected people, and these are just the beginnings of what would amount to almost a wholesale revision of American society, with its attendant, stupefying costs.
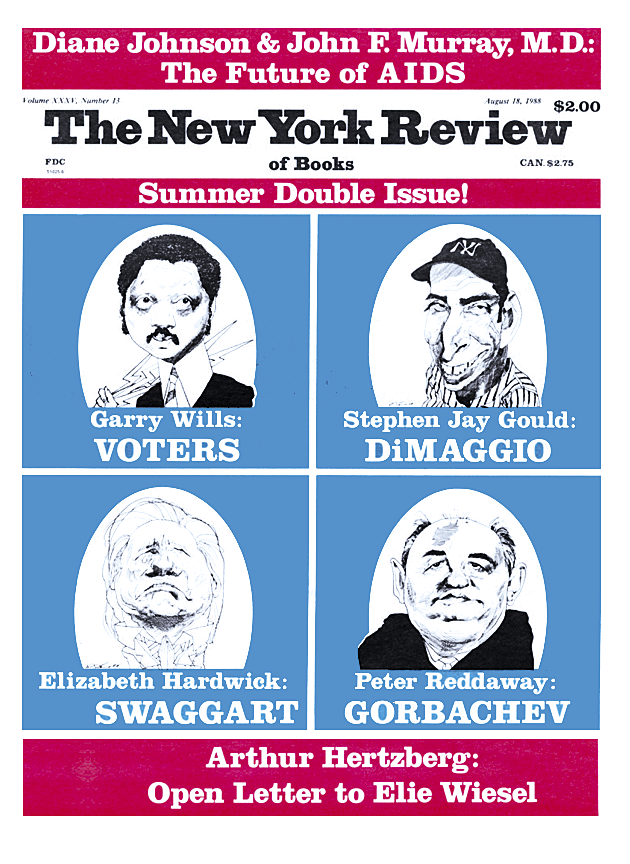
This Issue
August 18, 1988
-
1
Interview by Andrew Moss, University of California, with William Darrow, the author of an early cluster study of AIDS cases. An article in October, No. 43 (Winter 1987), suggests Dugas did not know he was infected. ↩
-
2
Interview with R. Chaisson, M.D., University of California, San Francisco, Audio Epidemiology Unit. ↩
-
3
Simon and Schuster, 1986. ↩
-
4
Shilts, p. 224. ↩
-
5
Shilts, p. 540. ↩
-
6
The Washington Post (June 23, 1988). ↩
-
7
N.A. Hessol et al., Presentation at the Twentieth Annual Meeting on the Society for Epidemiological Research, University of California, San Francisco (June 17, 1987). ↩
-
8
J.W. Curran, Science, Vol. 239 (February 5, 1988), p. 610. ↩
-
9
The WHO statistics indicate 100,410 reported cases of AIDS as of June 30, 1988. ↩
-
10
N. Nzilambi et al., “The Prevalence of Infection with Human Immunodeficiency Virus over a 10-year Period in Rural Zone,” New England Journal of Medicine, Vol. 318 (February 4, 1988), pp. 276–279. ↩
-
11
J.M. Mann, T. Quinn, H. Francis, et at., at the Second International Conference on AIDS, Paris, June 23–25, 1986; William Shack, personal communication, Department of Anthropology, University of California, Berkeley; Nancy Padian, et al., University of California, Berkeley, Department of Public Health. ↩
-
12
N.S. Padian, “Heterosexual Transmission of Acquired Immunodeficiency Syndrome,” in Review of Infectious Diseases, Vol. 9 (September–October 1987), pp. 947–960. ↩
-
13
William Booth, Science, Vol. 239 (January 15, 1988), p. 253. The CDC derived the number of cases in the US by multiplying the estimated number of persons in the various risk groups by an estimated average percentage for seropositivity in each group; because neither the number nor the average value is known with precision, considerable uncertainty remains about the true prevalence of HIV infection here or anywhere else. But the CDC estimate is based on more careful epidemiological methods than the 3,375,000 derived by Masters, Johnson, and Kolodny in their book Crisis: Heterosexual Behavior in the Age of AIDS. Their number was obtained by multiplying the number of cases in the US in late 1987 (approximately 45,000) by seventy-five (chosen from the inacurate assumption that for every AIDS victim there were fifty to one hundred HIV carriers). By that reasoning, there would now be approximately 4.3 million HIV cases. Masters, Johnson, and Kolodny also assert that “the AIDS virus is now running rampant in the heterosexual community” in the US, a conclusion even their own evidence does not support at this time, and an extravagance that could seem to call into question some of their sensible cautions about careful choice of sexual partners and use of condoms. ↩
-
14
Science, Vol. 238 (November 6, 1987), p. 747. ↩
-
15
Before getting one of the diseases such as pneumocystis pneumonia that define a diagnosis of AIDS, a victim can experience other complications that, when they include swelling of many lymph nodes, fever, weakness, and weight loss, have been called ARC, or AIDS-related complex. But the CDC has stopped using the term ARC and now includes the wasting syndrome in its definition of AIDS. ↩
-
16
Ranki et al., The Lancet, Vol. 2 (September 12, 1987), p. 589. ↩
-
17
J.W. Ward et al., The New England Journal of Medicine, Vol. 318 (February 25, 1988), pp. 473–478. ↩
-
18
N.A. Hessol et al., Third International Conference on AIDS, Washington D.C. (June 1, 1987). ↩
-
19
K-J. Lui et al., Science, Vol. 240 (June 3, 1988), p. 1,333. ↩
-
20
The New York Times (November 30, 1987). ↩
-
21
Confronting AIDS: Update, 1988 (National Academy Press, 1988). ↩