After twenty-three years of intense research into the human immunodeficiency virus (HIV), together with the accumulated experience of more than twenty million deaths from the in-fection worldwide, there is still no prospect of a vaccine to prevent AIDS. Is the discovery of a vaccine simply a matter of time? Or has this virus presented scientists with a hitherto underestimated, perhaps even impossible, challenge?
The International AIDS Vaccine Initiative (IAVI), the world’s largest single organization devoted to finding an AIDS vac-cine, has argued that the obsta-cles to progress are clear and resolvable—lack of political commitment and inadequate scientific resources. With offices in New York, Amsterdam, Nairobi, and New Delhi, it has invested $100 million in the search for a vaccine. At the Bangkok AIDS conference held in July of this year, Seth Berkley, IAVI’s president, argued that “only a vaccine can end the epidemic,” that “a vaccine is achievable,” and that spending on vaccine research must double to $1.3 billion annually in order to find it. “The world is inching toward a vaccine, when we should be making strides,” he said. The present situation was little short of “a global disgrace.”
But contrary to the predictions and promises of most AIDS experts, the signs are that a vaccine to prevent HIV infection will not be found for, at the very least, several decades to come—if at all. Those responsible for carrying on the global fight against AIDS do not accept this grim outlook, at least publicly. Yet it is a conclusion, based on all the evidence gathered so far, which increasingly defies rebuttal. Until the gravity of this scientific failure is openly acknowledged, a serious debate about how to end HIV’s lethal grip on some of the poorest and most vulnerable human populations in the world cannot take place.
1.
The holy grail of AIDS prevention is a single-dose, safe, affordable, oral vaccine that gives lifelong protection against all subtypes of HIV. The first hurdle facing vaccine designers, therefore, is dealing with the extraordinary genetic complexity of the HIV epidemic.
HIV exists as two strains—HIV-1, which dominates the epidemic, and HIV-2, which is largely confined to West Africa. So far, at least ten different patterns of HIV-1 infection have been identified. These patterns reflect particular geographic and genetic profiles of viral spread. For example, HIV-1 subtype B (there are nine genetic subtypes) is the common form of the virus in North America and Western Europe. India, by contrast, is under threat from HIV-1 subtype C. In Africa, where some two thirds of those with HIV now live (about 25 million people) and where there were three million new infections in 2003 alone, the situation is more diverse. Southern and eastern regions of the continent face a predominantly HIV-1 subtype C epidemic. Central Africa sees a highly mixed picture—HIV-1 subtypes A, D, F, G, H, J, and K. The implications of these differences for vaccine development remain uncertain. The best guess is that the genetic complexity of HIV will influence the effectiveness of any tested vaccine.
There are also over a dozen virus variants, called circulating recombinant forms, whose genomes have a structure that lies in between those of known subtypes. They also contribute to the difficulty of creating a one-size-fits-all vaccine. At present, scientists do not know if each subtype and every variant will need its own specific vaccine. It may well be that they will.
Worse still, a given subtype of the virus does not stay the same. HIV is continually evolving. The ingenuity of the virus in adapting to prevailing pressures in its environment—such as the existence of a vaccine that triggers an attempt by the human body to eradicate it—is owing to an enzyme called reverse transcriptase. This enzyme is essential for viral replication but it makes mistakes as it goes about its work. These mistakes, together with an extremely high rate of virus production, help HIV to produce an enormous family of genetically varied offspring.
Even if a vaccine were available, these different forms of HIV would almost certainly allow some of the virus to “escape” from any protective immune response that the human body mounted against it after vaccination. Some of these randomly generated “escape mutants,” as they are called, would then be selected for survival in succeeding generations of the virus, since they would possess the advantage of being “fitter”—avoiding the body’s immune response—than their nonmutated counterparts.
These problems become easier to understand when one considers how a vaccine to prevent HIV infection would have to work if it was to produce what experts call sterilizing immunity—that is, complete protection from infection. The normal immune system has two ways of responding to infection. The first depends on the antibodies we all produce in our bodies. These large molecules bind to the virus particle and neutralize it, preventing HIV from going on to infect human cells. There are two critically important proteins on the surface of HIV-1, which are called gp120 and gp41. They are the means by which the virus enters human cells and they are the main targets of the neutralizing antibodies. The difficulty is that crucial parts of these surface molecules are hidden from the attacking antibodies. Such resilient viral topography, together with several molecular tricks that enable HIV to evade human defenses, severely weakens the body’s immune response. Antibodies alone are therefore very unlikely to protect us from HIV.
Advertisement
The second response of the immune system involves not the production of antibodies but the rallying of cells to combat infection. There are two types of blood cell that are involved in an effective immune response to HIV—CD4+ and CD8+ T-lymphocytes, cells that develop within the thymus gland. The CD4+ cell is HIV’s primary target. It is this cell type that is hit hardest by the virus, causing the typical immunodeficiency that characterizes AIDS. CD8+ cells—also called cytotoxic T-lymphocytes (CTLs)—matter because, among other actions, they kill cells that become infected with HIV. They are usually assisted in their task by CD4+ lymphocytes, which are, appropriately, also known as T-helper cells. This mopping-up operation has the potential to damp down the damage that HIV can do to the body.
Once a person is infected, a contest begins between the virus, which is trying to establish a foothold in the body, and the cellular immune response, which is trying to stop the virus from doing so. A vaccine should tip the balance of this contest in favor of the immune system by increasing the numbers of CD4+ and CD8+ cells that are poised to swing into action if HIV gains entry to the body at some point in the future.
In truth, a vaccine that strengthens this kind of cell-mediated immunity would probably not prevent infection. It would likely slow the rate at which the virus took over and destroyed the body’s immune system; and such control of viral replication would be immensely helpful if it could be achieved. Indeed, the notion of a CTL-based HIV vaccine is surprisingly popular in view of the technical difficulties of producing it. David Garber and Mark Feinberg, respected HIV investigators at the Emory Vaccine Research Center in Atlanta, write:
If widely implemented, such vaccines may have a significant impact on improving the quality and length of life for HIV-infected individuals, while at the same time reducing the rate at which HIV continues to spread throughout the human population.1
But despite the importance of these T-cell responses against HIV, especially in the acute phase of infection, they ultimately fail to control HIV’s effects. Nobody knows exactly why. It is clear that a CTL-based HIV vaccine would have to improve upon the immune response that is induced by natural infection. This is a huge demand to put on a vaccine and it is far from clear that it could be achieved. Vaccines of this kind would face the additional problem of overcoming HIV’s remarkable genetic diversity.
The sum total of our knowledge about the genetics, biology, and geographical distribution of HIV indicates that vaccine scientists may have met their match in this adaptable foe. The reality seems to be that a vaccine against AIDS is becoming little more than a pipe dream.
2.
Despite these sobering concerns, the rhetoric surrounding AIDS vaccines continues unabated. At the Bangkok AIDS conference this July, for example, IAVI’s publication Scientific Blueprint 2004 strongly advocated the acceleration of global efforts to discover an AIDS vaccine. It deplored the fact that less than one percent of all health product research and development spending is currently allocated to finding a vaccine to prevent HIV infection. But IAVI is less clear about how the new money it is demanding—$650 million—should be spent.
The IAVI’s position is troubling. It raises the expectation that if only enough money were thrown into AIDS vaccine research, then a solution would appear in the not too distant future. But the implication that money is by itself the answer is wrong. The difficulties facing vaccine researchers are far more complex.
Meanwhile, in June of this year, at its Sea Island Summit, the G8 nations endorsed the creation of a new consortium—the Global HIV Vaccine Enterprise. It remains unclear exactly what this new organization will do.2 Such lack of clarity did not stop Lee Jong-wook, the World Health Organization’s director-general, from calling it “a new political and financial dimension” to HIV vaccine development. It is neither political nor financial.
There is talk of greater scientific collaboration, along the lines of the Human Genome Project. The words “strategy” and “synergy” are often mentioned in documents discussing the enterprise, words that certainly indicate good intent. For example, the UK government’s program for tackling HIV and AIDS in the developing world, which was published shortly after the Bangkok meeting, makes the unqualified comment that the enterprise “will accelerate research and development of an effective vaccine.” But so far the enterprise has no formal organization, no overall leadership, and no new money for research—just a $15 million start-up grant to create a “virtual center,” which will likely be located in an already existing American institution.
Advertisement
One reason why scientists created IAVI in 1996 and lobbied for the Global HIV Vaccine Enterprise in 2004 was a sense of collective failure to deliver on earlier commitments to develop a vaccine. Since 1987, there have been over eighty trials of thirty different candidate AIDS vaccines. All have proven to be disappointing. The results of the world’s first two large-scale vaccine studies were reported in 2003. Again, both failed to show any benefit. Given these early disappointments, what can we expect from HIV vaccine research in the future?
The perfect vaccine would be a live but inactive or attenuated version of HIV—that is, a virus which has been disabled and cannot cause disease. This type of vaccine would resemble those already used to prevent polio, measles, and yellow fever. Indeed, the vaccine that eradicated smallpox was a live but attenuated form of the smallpox virus. But the great anxiety about a live attenuated HIV vaccine is that it would be unsafe. Since there is a small possibility that the vaccine could cause the infection it was trying to prevent, the risk, as of now, is simply too great to take.
The alternative low-risk strategy is to use a vaccine made up of dead protein. For example, if preparations of the proteins gp120 or gp41 were injected, there would be no opportunity, even accidentally, to cause HIV infection. The proteins generate an immune response within the human body that scientists had once hoped would resemble the immune response generated by HIV itself. This approach was the basis for the two failed trials of gp120-based vaccines in the US and Thailand, reported last year.
Between these two unworkable extremes, there is a multiplicity of new technologies that are now being tested. The idea behind most of these approaches is to deliver a vaccine consisting of protein or DNA using a live virus that is not HIV. This live virus acts as a vehicle—called a vector—to carry and enhance the effectiveness of the vaccine. More importantly, instead of trying merely to generate antibodies to bits of HIV, such as gp120, the intention behind using a live virus is to activate the T-cells that are used by the immune system as one of its main responses to infection. These vaccines aim to produce cytotoxic T-lymphocytes that will kill HIV-infected cells. But already this approach represents an important concession by vaccine scientists. For instead of pursuing the goal of preventing HIV from infecting the body (achieving immunity through a process of sterilization), a vaccine strategy based upon cell-mediated mechanisms acknowledges that the best that can be hoped for is a vaccine to suppress an already established infection.
One such CTL vaccine is currently being studied in Thailand. Sixteen thousand men and women are being recruited for a three-year trial of a gp120 vaccine whose effects will, it is hoped, be boosted by a viral vec-tor called canarypox. Four injections of the vaccine will be given. Few scientists expect this study to yield a breakthrough. Indeed, many experts believe that the Thai trial is misjudged, even unethical. The vaccine vector is a weak stimulant of the immune response. One part of the vaccine is completely ineffective. And there is no evidence that the vaccine will do what it is supposed to do—namely, provoke protective antibody and cellular responses to HIV. In view of these deep concerns, plans for undertaking a similar study in the US have been rejected. Scientists simply do not believe that the evidence supporting the vaccine’s efficacy is sufficient to justify such a large-scale investigation among human beings. The final results of the Thai trial will not be available until 2008 or 2009. It is a long time to wait for failure.
Later this year another viral vector, this time using a virus called adenovirus, will enter advanced clinical testing. Scientists see this study as a useful step in proving that the concept of a viral vector works, but nobody expects this vaccine to prevent HIV infection.
A further approach is to introduce into the human body naked DNA—HIV genes that are sown into a circle of harmless bacterial DNA. DNA vaccines were initially hailed as a revolution in vaccinology. That exuberance was based on very preliminary findings in mice. This premature enthusiasm has more recently given way to caution as the technology has gradually been transferred to humans, with only limited short-term success.3 Finally, since HIV usually enters the body through mucosal surfaces—the vagina and rectum—augmenting an immune response at these portals of entry by using what scientists call mucosal AIDS vaccines might be an additional way to improve protection against infection. Several vaccine candidates exist, but human studies have only recently begun. Experts disagree about whether this technique will offer any advantages over more conventional vaccines.
Currently, there are twenty-two candidate AIDS vaccines undergoing human trials. Although this number has risen sharply—there were only seven vaccines being tested in 2002—they do not exhibit a conceptual leap in overcoming the obstacles to a vaccine I have outlined. Still, it is fair to say that the science of why vaccines fail is progressing at a rapid rate. But here lies a moral rather than a scientific predicament for doctors looking after people with AIDS.
When a clinical trial of a vaccine begins, scientists hope that the study will add useful information about the efficacy of the vaccine and its mechanism of action. Ideally, they start from a position of neutrality—scientists call it the “uncertainty principle”—about whether the technology being tested will work or not. They might hope that it will, but they honestly do not know for sure. Yet the pace of HIV vaccine research is now growing so swiftly that the scientific goal of conducting and completing a clinical trial may be threatened by a higher ethical obligation—to inform those taking part in the study that the original scientific basis for the research may have been modified by later work. Or it may even have been completely discredited. At this point, the trial should be stopped—and stopped quickly. No human experiment ought to continue if its scientific justification has been undermined.
Many scientists believe that the Thai HIV vaccine trial, which had recruited over 2,500 of its projected 16,000 participants by June 2004, has no chance of success.4 Yet the investigators overseeing the study (who include American scientists), the local Thai institutional review boards, and the Thai Ministry of Health have all remained silent—at least on the record. Off the record, one member of the study’s safety committee smiled anxiously when I asked him about the propriety of continuing this trial. “Good question,” he shot back. It seems that what is unacceptable in the US is now somehow acceptable in Thailand. This smacks of astonishing ethical relativism.
IAVI is correct, therefore, to describe the present landscape of vaccine research as a “tragedy.” But it is tragic not because insufficient time or resources have been brought to bear on the problem. A vast amount of very good scientific work has been completed on the biology of HIV and the various avenues open for vaccine development. Rather, what is tragic is the inclination of the HIV vaccine community to portray the future of vaccine research in such a misleadingly hopeful light—to support research at any moral cost.
3.
What is the alternative to a vaccine? There are two widely heard answers to this question, which unnecessarily compete with each other—expanded access to treatment and a great many proven and yet-to-be-proven preventive measures. Lee Jong-wook’s ambitious target of treating three million people with anti-HIV drugs by the end of 2005—his so-called “3 by 5” program—is so far falling very short of expectations. Although twice as many people are now being treated with drugs than in 2002, the present number—about 440,000—is still 60,000 short of WHO’s projections. The agency admits that this situation is “disappointing.” Some reports have gone further, drawing attention to experts who accuse WHO of “sloppy” statistics in their claims for even limited success.5
Prevention efforts have largely rested on the formula of A-B-C—abstinence from sex, being faithful, and using condoms. While these messages are important, for many people they are very difficult or impossible to put into practice. The most disturbing aspect of the HIV epidemic today is the way in which it is spreading among women. Women make up almost two thirds of fifteen-to-twenty-four-year-olds living with HIV—they are now three times more likely to become infected than young men. Over three quarters of these HIV-positive women live in sub-Saharan Africa—in South Africa, one in four becomes infected with HIV by the time she is twenty-two years old. In 1985, 35 percent of those with HIV were women. By 2003, that proportion had climbed to 48 percent. In sub-Saharan Africa it is 57 percent. Even in North America, the prevalence of HIV among women rose by 5 percent between 2001 and 2003—the highest increase among women in any part of the world today. Why is this?
Partly, it is because of lack of knowledge about the virus and its transmission. Partly, it is because women are more vulnerable to infection than men. For example, the risk of acquiring HIV for men engaging in peno-vaginal sex is 3 per 10,000 contacts. For women, it is 20 per 10,000 contacts, a sevenfold increased likelihood of infection. But more importantly it is because of the kind of relationships that women have with men. Many women are simply not in a position to negotiate A or B or C with their male partners. Older men will frequently have sex with younger women who are not in a position to refuse them. Migration of men in the pursuit of work or war encourages multiple sexual partners and unsafe sexual practices. And the concurrent epidemic of sexually transmitted infections only increases the risk of acquiring HIV still further. These facts are frequently ignored by many Western policymakers seeking simple, all-encompassing solutions.
What might help women most of all is a personal method that they could use to protect themselves from infection. If a condom is neither available nor practicable, could a substance applied to the vagina which destroys the virus—a microbicide—be the answer? Some scientists believe so. Dr. Zeda Rosenberg, who leads the International Partnership for Microbicides, argued in Bangkok that a microbicide to protect women from HIV could be available within five years. One hopes that this prediction does not go the way of those made about vaccines.
It is not surprising that the debate about the best means to combat the global AIDS epidemic has also become a domestic political issue in the US. The President’s Emergency Plan for AIDS Relief (PEPFAR) will invest $15 billion in AIDS treatment, prevention, and care programs over five years. Fifteen nations have been chosen to be beneficiaries of PEPFAR.6 The plan is being administered by Randall L. Tobias, the former president and chief executive officer of Eli Lilly.
Bush’s cash commitment has been welcomed by people in the AIDS community. But many are disappointed that the US is not intending to provide greater support to the only international financing organization devoted to building AIDS prevention programs in the countries that need them most. This Global Fund to Fight AIDS, Tuberculosis, and Malaria was created in 2002, having been endorsed by the UN, together with the leaders of G8 and African nations. After only thirty months it had spent over $3 billion on almost three hundred two-year programs in nearly 130 nations.7 Of the US government’s $15 billion, only $1 billion is being channeled to the Global Fund over five years.
To have made such a relatively small investment is to have missed an important opportunity. The Global Fund was created specifically to meet the needs of those most at risk of AIDS. Duplicating its efforts with an exclusively American initiative will waste time and resources. There is also a suspicion that PEPFAR will allow the US government to pursue its own narrow ideological agenda—for example, by supporting faith-based abstinence efforts rather than programs for reducing harm through campaigns for needle exchange and condom distribution.
While speaking about his plans in Philadelphia in June of this year, Bush underlined the “moral message” of PEPFAR. He said that “we need to tell our children that abstinence is the only certain way to avoid contacting HIV.” John Kerry has responded by promising to double the amount government spends on AIDS and to work more closely with multilateral organizations such as the Global Fund. AIDS has become a deeply partisan issue in an election year.
Amid this polarized debate, vaccines are barely mentioned. In UNAIDS’s two-hundred-page global report on the epidemic, released in July, vaccines received only a cursory reference. Elsewhere, however, UNAIDS reiterated IAVI’s conclusion that investment in vaccine research is falling well below what is needed. In Bangkok, some delegates deplored the failure to subject the lack of progress toward an AIDS vaccine to critical scrutiny.8 José Esparza, a leading HIV vaccine advocate and an adviser on vaccines to the Bill and Melinda Gates Foundation, was frank in saying “we were wrong” to think that a vaccine could be discovered easily.9
And yet the notion of a vaccine has not been entirely forgotten. A new kind of vaccine has been proposed, one that many observers believe has had a profound effect in a country long threatened by HIV. In describing how Uganda responded to AIDS in the 1980s, President Yoweri Museveni argued that “with no medical vaccine in sight, behavioral change had to be our social vaccine and this was within our modest means.” He gave this comparison:
Individual behavior and personal responsibility, based on knowledge, will be our best protection against AIDS and other future epidemics. In Uganda we managed to bring the HIV sero-prevalence from 18.6 percent to 6.1 percent using just a social vaccine, a reduction close to 70 percent…. I am told by the medical scientists that a medical vaccine with 80 percent efficacy is considered a very good vaccine.
As Helen Epstein has recently pointed out, however, the relatively stable family environment in Uganda is significantly different from more violent and migratory conditions seen elsewhere in Africa:
Ugandans are more likely to live near their families and know their neighbors, and this probably enabled a more compassionate, open response to AIDS and a more rapid acceptance of the idea that trust and mutual fidelity were possible. The far more brutal history of southern Africa had the opposite effect. It weakened people’s sense of trust and undermined relationships between men and women. Many experts contend that sexual-behavior change in Africa is complicated because women’s fear of abusive partners inhibits private discussions of sex, condom use and HIV.10
In view of the different social conditions in different regions it is often far from clear just what a social vaccine would consist of and how men and women would accept it. In Bangkok, the Thai government pledged its commitment to sex education in schools and behavior change, explicitly endorsing the notion of a social vaccine.11 But one wonders just how efficiently particular programs of sex education in schools will change behavior. To find the best means of preventing HIV, we need evidence on a country-by-country basis about what methods do and do not work in different social environments. For most parts of the world, that evidence does not exist. What is perhaps striking is the way in which the word “vaccine,” embodying a particular idea that remains unfulfilled in one context, is being applied in another setting. It seems that the concept of a vaccine is too powerful, its connotations offer too much hope, to let technical failure in the laboratory extinguish its meaning for communities.
Six days of talking in Bangkok made it clear that the world should plan its response to AIDS on the assumption that there will be no vaccine, in the ordinary sense of the word, to stop the spread of HIV. Microbicides might eventually be part of the answer, as might A-B-C. But our long-term defense requires a deeper understanding of the conditions in which AIDS is transmitted, and how they might be changed. The most important recent revelation about HIV-AIDS—but the one most difficult to act on because it does not lend itself to a simple technical fix—is the central position of women in the epidemic.12 For it is the relations of women with men in different societies that will determine the course of this plague.
AIDS is increasingly affecting women; and marriage—in which there can be frequent episodes of male violence and sex with multiple partners—has become a serious and significant risk factor for acquiring HIV.13 In Uganda, for all its relative progress, rape and domestic abuse have been important factors in sustaining the epidemic.14 Is it too much to hope that the searing catastrophe of AIDS may have put before women and men an issue that they can use to confront male violence, exploitation, and stigma? By 2010 there will be 25 million children orphaned because of AIDS. This is a human atrocity that women and men must contend with together—and without the help of a vaccine.
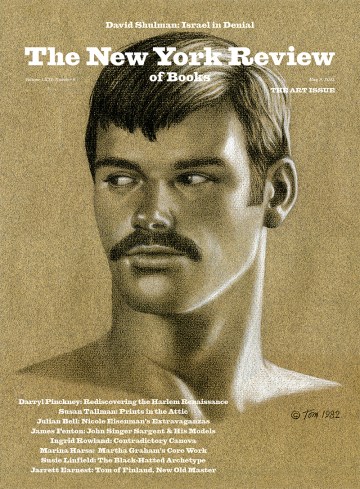
This Issue
September 23, 2004
-
1
See David A. Garber and Mark B. Feinberg, “AIDS Vaccine Development: The Long and Winding Road,” AIDS Reviews, Vol. 5, No. 3 (2003), pp. 131–139. ↩
-
2
The idea for a Global HIV Vaccine Enterprise was first raised in 2003 by leading representatives of the Bill and Melinda Gates Foundation, the National Institutes of Health, the Centers for Disease Control and Prevention, UNAIDS, and IAVI. The proposal gave details about structures and standardizations for laboratories, clinical trials, and manufacturing. There was an implicit assumption, nowhere argued cogently, that the science will one day deliver a vaccine. See Richard D. Klausner and colleagues, “The Need for a Global HIV Vaccine Enterprise,” Science, Vol. 300 (2003), pp. 2036–2039. ↩
-
3
See Marie J. Estcourt and colleagues, “DNA Vaccines Against Human Immunodeficiency Virus Type 1,” Immunological Reviews, Vol. 199 (2004), pp. 144–155. ↩
-
4
In January 2004, a group of respected investigators wrote to Science voicing their concern about the wisdom of the US government in sponsoring the Thai vaccine trial. They did not believe that the vaccine had any prospect of success. They suggested that “one price for repetitive failure could be crucial erosion of confidence by the public and politicians in our capability of developing an effective AIDS vaccine collectively.” See Dennis R. Burton and colleagues, “A Sound Rationale Needed for Phase III HIV-1 Vaccine Trials,” Science, Vol. 303 (2004), p. 316. ↩
-
5
See Lawrence K. Altman, “Ambitious HIV Plan Slowed by Obstacles,” International Herald Tribune, July 12, 2004, p. 3. ↩
-
6
These countries are Botswana, Côte d’Ivoire, Ethiopia, Guyana, Haiti, Kenya, Mozambique, Namibia, Nigeria, Rwanda, South Africa, Tanzania, Uganda, Vietnam, and Zambia. ↩
-
7
Tuberculosis is the most common additional infection among people living with HIV. It causes up to 40 percent of deaths in those with AIDS. ↩
-
8
See Moyiga Nduru, “Loud Silence on AIDS Vaccine Angers Some Researchers,” Terraviva, July 13, 2004, p. 3. ↩
-
9
Anthony Fauci, the influential and respected director of the US National Institute of Allergy and Infectious Diseases, has called HIV a “very special virus.” He was unusually candid in a little-reported interview he gave to a magazine distributed in Bangkok. Fauci was asked whether it was conceivable that a vaccine to prevent HIV infection might never be developed. He replied, “I think that’s possible…. All of us are working under the assumption that we will, but there’s certainly the possibility that we’re not going to be able to develop a truly effective preventive vaccine.” See International Antiviral Therapy Evaluation Center Update, July 2004, p. 19. ↩
-
10
See Helen Epstein, “The Fidelity Fix,” The New York Times Magazine, June 13, 2004. ↩
-
11
See Preeyanat Phanayanggoor, “Social Vaccine Scheme to Give Better Sex Education in Schools,” Bangkok Post, July 13, 2004, p. 2. ↩
-
12
The report Women and HIV/AIDS: Confronting the Crisis was released in Bangkok and jointly produced by UNAIDS, the UN Population Fund, and the UN Development Fund for Women. ↩
-
13
See Kristin L. Dunkle and colleagues, “Gender-based Violence, Relationship Power, and Risk of HIV Infection in Women Attending Antenatal Clinics in South Africa,” The Lancet, Vol. 363 (2004), pp. 1415–1421. ↩
-
14
See Anne-Christine d’Adesky, Moving Mountains: The Race to Treat Global AIDS (Verso, 2004). ↩