Few of us lose a parent without regret and some self-reproach, some sense of things undone or injustices unredressed; it is a natural component of grief. The literature of memoirs by children of their parents, from Father and Son to Mommie Dearest—whether by Edmund Gosse or John Stuart Mill, Sean Wilsey or Francine du Plessix Gray—may be affectionate, angry, or ambivalent, but such works inevitably contain conscious or unconscious expressions of the reservations and differences essential in a parent–child relation if the child isn’t to be submerged in the parent’s tremendous identity. David Rieff’s memoir of his mother, Susan Sontag, has all of these qualities, which perhaps accounts for its power beyond mere eulogy, elegy, or complaint.
Swimming in a Sea of Death is narrowly focused on his reaction to her death in 2004 from a rare blood malignancy, and on the medical issues around it, some of which she had also written about, though only very generally, from the point of view of a cancer survivor. Rieff now gives his account of her nearly thirty-year battle against three potentially fatal cancers, and its effect on him. Besides being an eloquent record of grief, it raises a number of issues pertaining to cancer, its treatment, and our attitudes toward the language of illness and dying—subjects long of interest to Sontag herself.
1.
In 1975, Sontag, then aged forty-two, was diagnosed with stage-four (advanced), metastasized breast cancer. Doctors explained the “hopeless” prognosis to Rieff, then twenty-three, but she herself was not directly told the medical facts, a reticence common at the time. One can be sure, however, that she knew the grim statistics perfectly well, because she looked them up. In her famous essay “Illness as Metaphor,” first published in these pages in January and February 1978, and later as a book with “AIDS and Its Metaphors,”1 she says:
All this lying to and by cancer patients is a measure of how much harder it has become in advanced industrial societies to come to terms with death. As death is now an offensively meaningless event, so that [cancer] widely considered a synonym for death is experienced as something to hide.
She herself was no exception to this reluctance: Rieff emphasizes that she hated talking about death and “loved living,” had an “avidity” for life. Her unwillingness to accept her own mortality continued onto her deathbed, and Rieff didn’t dare bring it up, a fact that most curiously reflects his own ambivalence about her attitude toward illness. Her denial of impending death, which he wished to respect, versus his sense of what she should know, discuss, face, and accept, is one of the themes of his book. Another is the language of such discussions, and the sincerity with which it is deployed, which was central to Sontag and Rieff’s experience with doctors; and the last is the larger metaphysical question, and
in the end, that is the question that haunts me. Had Stephen Nimer [Sontag’s last physician] been able to save my mother’s life, would she have been reconciled to dying of something else later on? Are any of us, when it’s our turn?
Sontag had declared when she was a sixteen-year-old student at the University of Chicago that death was not going to cut her own life short, an interestingly precocious preoccupation at an age when people normally sense themselves immortal. She wrote then of “not being able to even imagine that one day I will no longer be alive.” It was the start of her commitment to do whatever it took to live: dying was not an option. “The simple truth is that my mother could not get enough of being alive. She reveled in being; it was as straightforward as that,” Rieff says.
Her breast cancer in 1975 was the first test of her resolve. It had been shown to have already spread to lymph nodes in her armpit, a combination considered hopeless by most cancer authorities of the day. Today’s fairly standardized treatment for breast cancer consists of minor, individualized variations of three major means of attack: local surgery, regional radiation, and systemic chemotherapy; but the treatment options for Sontag at the time were limited to surgical removal of the breast—a mastectomy, either radical or limited—and a course of primitive palliative chemotherapy. (Radiation was available, but we aren’t told if it was considered in her case.) Chemotherapy, which today would be given without hesitation to a woman with a cancer similar to Sontag’s, with full expectation of a remission and extension of life measured in months or even years, was then in its infancy.
Radical mastectomy was still in vogue, although its efficacy compared with alternative, more conservative surgical approaches was being evaluated. (Studies would prove it unnecessarily drastic.) The brutal operation, now obsolete, consisted of complete removal of the entire affected breast, plus the large pectoral muscles underneath on the outer surface of the rib cage, and all the lymph nodes and other tissues extending up to and deep within the armpit. Radical mastectomy regularly left a disfiguring concavity on the upper half of one side of the chest plus a weakened swollen arm on the same side, but it remained the standard breast cancer treatment for almost a century. In Annie Leibovitz’s 1992 photographs, Sontag, otherwise naked, covers her mutilated chest, the gesture an emblem of the trauma of this disfiguring operation.
Advertisement
Before the surgery at Memorial Sloan-Kettering Cancer Center in New York City, she went to the Cleveland Clinic for a second opinion; we don’t know what she was told about chemotherapy, but she was counseled to have a limited rather than a radical mastectomy—advice she disregarded, opting for the more mutilating procedure as soon as she returned to Sloan-Kettering. Rieff explains that Sontag’s choice was totally consistent with her determination to do anything and everything possible to survive: “Real commitment for her,” like the type of mastectomy she elected to have, “was always radical.”
Where many might have accepted the finality of her bleak prognosis, she took matters into her own hands, read up on her condition, and with help from a French friend (the actress Nicole Stéphane) contacted a French physician, Lucien Israël. Israël was originally a lung specialist who had switched to oncology before the specialty was officially recognized in France, and was known for his encouraging results in her sort of case using experimental immune therapies and chemotherapeutic agents not then being used in the US. In the 1978 English translation, entitled Conquering Cancer,2 of his 1976 book, Le Cancer aujourd’hui, which must have been mostly written before he treated Sontag, the pioneering Israël said, “In the last few years, disseminated breast cancer has entered the ranks of cancers that can be controlled and perhaps cured.” Sontag wasn’t getting that message in America.
In response to inquiries, Israël replied that he thought her case not hopeless, and she started treatment—painful and problematic immuno-chemotherapy, then fairly new, some of which was received in France, some at Sloan-Kettering using Israël’s “cocktail.” One may suppose that Sontag’s familiarity with French and France made her more comfortable with seeking treatment in a foreign country than most Americans would have been. She was then “cured” (it is a term Israël himself later dislikes) for over twenty years, only to be struck with another cancer, this time of the uterus.
Dr. Israël is perhaps best known as a champion of immunotherapy—the administration of certain substances, often (in the Seventies) killed bacteria or their products—in an effort to revitalize an immune system overpowered by the effects of chemotherapy or the cancer itself. In the long run, immunotherapy hasn’t turned out to provide the clinical boost that Israël envisioned, but remains a subject of considerable current research interest.3 Israël was also among the first to use and extol the superior benefits of cancer chemotherapy with multiple rather than single powerful agents: currently, most aggressive chemotherapeutic regimens include multiple drugs, though the “maintenance treatment” subsequently given sometimes uses only one. Sontag’s admiration for Israël is evident in the blurb she wrote for Conquering Cancer: “By far the most intelligent, informative and useful book ever written on cancer.”
Sontag received combined immuno-chemotherapy. (Her enthusiasm for immunotherapy is apparent in Illness as Metaphor: “As chemotherapy is more and more supplanting radiation in the treatment of cancer patients, an effective form of treatment (already a supplementary treatment of proven use) seems likely to be found in some kind of immunotherapy.”) Sontag was a self-proclaimed risk-taker, and she sought treatment that differed from the standard regimens then available—on which the prevailing and forbidding statistical prognosis was based. Israël’s boundless optimism, plus his forceful and daring approach to treating cancer, especially breast cancer, were a perfect match for her determination and willingness to try anything to survive.
Her treatment was also radical, at least when compared with present-day, precisely regulated standards of experimental medicine, in that her therapeutic cocktail, brewed by Israël in France, was sent to New York City and administered twice weekly by physicians at Sloan-Kettering. Today, in the US, experimental drugs require rigorous and lengthy evaluation before they can be administered, and uncertified regimens would not be allowed. To bypass this process, especially to get unauthorized and usually futile treatments such as laetrile or krebiozen, cancer patients must travel outside the United States, to Mexico, for example.
Going outside the approved channels was in Sontag’s case an inspired decision, and she remained a convinced advocate of patients researching and reasoning on their own behalf. Her French adventure gained her more than twenty years. There are various explanations for her long survival that tend to discount the French treatment. Her friend Dr. Jerome Groopman, the expert oncologist and medical writer, explained to Rieff after she had died that “there are always people on the tail end of the [statistical survival] curve,” and that Sontag was one of them; others might declare her an “outlier,” off the curve entirely, or conclude that she still had residual cancer of which the metastases hadn’t yet cropped up (as sometimes happens). Both Sontag and Rieff, though, attribute her survival to Israël and his innovative treatment, and to her decisions, guided by her own perception that chemotherapy, with its systemic effects, would be better than focal radiation at attacking possible disseminated metastases.
Advertisement
It is worth noting that the controversial Israël had also annoyed many of his colleagues by constantly and publicly advocating cooperation among medical specialists, instead of the then-prevalent competition among surgeons, radiation therapists, and medical oncologists in the treatment of patients with cancer. As Israël pointed out, in the Seventies, the treatment you got depended somewhat on the specialty of the doctor you happened to see first. Today, just as he was urging then, multidisciplinary case conferences—tumor boards—are a regular feature in cancer centers.
Rieff, in Swimming in a Sea of Death, raises some important issues that pertain to contemporary medicine in general, not just to Sontag’s particular diseases. The five-year survival rate of women with breast cancer improved only slowly for a decade or so after 1975, when Sontag was first stricken, and then advanced substantially. But as he emphasizes, the concept of five-year survival can be misleading. If breast cancers are diagnosed, say by mammography, earlier than would once have been the case, five-year survival rates are bound to increase, even if nothing else changes, because a patient has been recruited into the medical system earlier than she would otherwise have been: what counts is the impact of early diagnosis on overall mortality, not just breast cancer mortality. (Radiation of breast cancer appears to hasten death from heart disease; Sontag’s death from myelodysplastic syndrome was caused by the cancer chemotherapy she had received. Such deaths would not be attributed to “breast cancer.”)
According to the latest Annual Report to the Nation on the Status of Cancer, 1975–2004,4 the annual incidence of breast cancer (the number of new cases per 100,000 women) decreased 3.5 percent per year from 2001 to 2004 (the last year covered by the report): “the first decrease observed in twenty years.” Mortality rates from breast cancer also decreased. But teasing out the reasons for these “favorable changes” is less exact than the numbers themselves. The most likely explanation for the decreased incidence appears to be decreased use of estrogen by post-menopausal women, whereas early diagnosis, improved treatment, and rigorous application of standardized therapy have all probably contributed to the reduction in mortality.
2.
All told, Susan Sontag had three different malignancies: the advanced cancer of the breast at age forty-two; then, twenty-three years later, sarcoma of the uterus, an unusual form of uterine cancer; and finally, myelodysplastic syndrome, a rare kind of malignant and usually lethal transformation of the bone marrow brought on, paradoxically, by the earlier chemotherapies that had unquestionably saved her life. The beginning of the end was announced on March 29, 2004, when Rieff accompanied his mother to her appointment with “Dr. A.,” whom he describes as an unfeeling physician. His lack of sensitivity, however, seems to have consisted in the coldhearted bluntness with which he gave them Sontag’s death sentence: she was, he told her, suffering from the myelodysplastic syndrome, “a particularly lethal form of blood cancer,” and, in response to her questions, he said there was little to be done. Before the visit, Rieff had already suspected that his mother was ill—a pastiness and pallor evident in recent photographs, the development of bruises all over her body—and he might have inferred it from the fact that she had already undergone a bone marrow biopsy, not a routine procedure, the results of which clinched the diagnosis Dr. A. was giving them.
In 1969, Elisabeth Kübler-Ross published her (now sometimes challenged) book On Death and Dying,5 in which she described the five stages that many ordinary people go through after learning that they have a fatal illness: denial, anger, bargaining, depression, and, finally, acceptance. Sontag, though, was not an ordinary person. Rieff tells us that denial didn’t play a role, but that she was stunned, physically overcome, and very likely angry. This was the third time she had been diagnosed with cancer and she was entitled to be angry, a reaction that she had earlier addressed in Illness as Metaphor: “Why me? (meaning ‘It’s not fair’) is the question of many who learn they have cancer.”
But she was constitutionally against bargaining and acceptance. After recovering from hearing Dr. A.’s death sentence, she began to plan how to stay alive.
Rieff, on the other hand, after having meticulously explained why his mother’s decision was inevitable, revisits it in anguish: “My failing was that my own ambivalence about the choice she had made often rendered me almost mute.” And: “Even now, I am astonished by the extent to which she succeeded. What I do not know is whether her success in this was a blessing or a curse.” He is almost the last person to accept that she could have known what she knew, and is reluctant to think of her inner state:
For the sake of her happiness, even of her sanity, I am glad she did not go further than she did in finding out what the state of play in cancer really was. The news was so terrible. The news is still so terrible. As I would find out. As she would find out.
3.
There have been a few striking successes in the treatment of specific malignancies—lymphomas, certain leukemias, and cancer of the testes, for example—which are all much less common than the “big-four” cancers of the lung, colon, breast, and prostate. But myelodysplastic syndrome was not among the conditions for which there was much hope. Sontag greatly admired Lance Armstrong’s remarkable recovery from an equally hopeless, widespread (brain, lungs) testicular cancer, crowned by seven consecutive victories in the Tour de France, probably the world’s most grueling sporting event, not all of which she lived to applaud.
She lost her battle with myelodysplastic syndrome but not without trying everything that medicine had to offer. The odds of her surviving were terrible, but couldn’t have been much worse than those governing her earlier breast cancer. There was a slim chance that, once again, she could beat the odds and end up on the tail end of the survival curve, and that slim chance was a stem cell (a special type of bone marrow) transplant at the best place in the world, according to her physician, Dr. Nimer: the Fred Hutchinson Cancer Research Center in Seattle. Sontag knew that a stem cell transplant was an enormously high-risk long-shot possibility, especially at her age (seventy), which—naturally for her—she enthusiastically embraced, despite warnings of the pain and suffering it entailed. Those who have seen Annie Leibovitz’s harrowing photographs of Sontag on her deathbed have seen all too clearly that her eventual suffering was enormous, and surely the source of much of Rieff’s ambivalence about her choice.
In general, though, we can’t ignore the fact that Sontag was privileged. She benefited from excellent physicians, enough money to pay for cutting-edge therapy not covered by insurance, and an indomitable determination to find the most advanced treatments available, all of which helped her survive two duels with often deadly malignancies, even if her final bout with myelodysplastic syndrome, a product, as we have seen, of the earlier chemotherapy that saved her life, proved too much for even the highest-quality expertise and treatment that contemporary medicine had to offer.
After Sontag’s death, Rieff wrote in The New York Times Magazine6 about some of its details that he does not repeat here, especially about the enormous cost of her final treatments. Dr. Nimer advised her to have the costly transplant, but payment for the procedure was denied by Medicare, her primary insurer; and although her other insurer agreed to pay for a transplant at one of four local hospitals, they were rejected (presumably by Nimer) as inexperienced and hence unsatisfactory. Resolute, she paid $45,000 to identify a compatible bone-marrow donor, and put down a deposit of $256,000 on admission to Hutchinson. We can only wonder how many other people—with the identical medical condition and therapeutic imperatives—would have been able to do the same, a point underscored by Rieff forcefully in the earlier New York Times Magazine piece, in which he draws attention to the inequities in American medicine: “I cannot honestly say that there was anything fair about [her treatment].”
Sontag’s experience reminds us that today, exactly as in centuries past, the most powerful determinant of health—whether measured in life expectancy, maternal mortality, childhood survival, or the incidence of tuberculosis—is wealth: the rich always fare better than the poor, even in countries where—unlike the United States—there are high-quality health care services available to everyone.
There are many other side issues about American medicine raised in Rieff’s short memoir, beginning with the fact that contrary to what most of us like to believe, but as Sontag’s experience showed, other advanced nations may be using therapies not yet available to us, and, almost more influential, may have therapeutic approaches or prejudices different from the prevailing American ones, which encourage or allow different and sometimes superior treatments. Sontag, in AIDS and Its Metaphors, and in person, was always emphatic that a patient has to take charge of his or her case, ask questions, read up on his condition, and seek out the right doctor or the right medical center, something objectively determinable from published statistics and papers:
Get the doctors to tell you the truth; be an informed, active patient; find yourself good treatment, because good treatment does exist (amid the widespread ineptitude).
4.
Related to all this is Rieff’s confession that “during my mother’s illness, I very consciously decided to take no notes.” That may be a suitable resolve for writers who want to look back unhampered by facts, but it is completely wrong for patients and their families and friends, as Rieff’s later dismay reflects: everyone should be armed with pad and pen and take notes on everything—and ask questions for clarification. Some oncologists recommend tape-recording such meetings. (Furthermore, between visits, when questions come to mind, patients should write them down and take them to the next appointment.) Many essential facts get overlooked or misconstrued by people facing stressful encounters in doctors’ offices. Sontag and Rieff had that exact experience, which he painfully describes, when Sontag is unable to remember later whether her blood had or hadn’t “converted” to a leukemic state, according to the doctor they had just seen.
In this connection, doctors advise that, ideally, in life-and-death situations such as Sontag was facing, when all the medical facts are known, thorough discussions should be held with family members and, if needed, with close friends or advisers, concerning the risks and benefits of the various treatment options, and then a decision should be arrived at, chiefly by the patient, obviously the one most involved. But thereafter, the family members and others, who had all had their say, should pitch in and support whatever the patient has decided: unambiguously, no matter which side they were on during the deliberations.
Sontag and Rieff seem to have had no such discussions: Sontag had clearly made up her mind since girlhood about exactly what she was going to do when a medical catastrophe arrived, and seems neither to have needed nor wanted any input. That Rieff seems to have had no role in making the crucial decisions in part explains his continuing anguish.
Another source of it is perhaps a matter of temperament. Her emphasis on truth-telling, and Rieff’s hesitancy about it, bring up the whole issue of the language of medical communication, one of the subtexts of the book. Almost anyone who has dealt with some grave medical situation will feel that doctors are either too frank or not forthcoming enough; and sometimes we feel both things at once. Rieff addresses this conflict without resolving it, but it underlies his sense of frustration after his experience left him convinced that Dr. A. was unfeeling: in speaking bluntly to Sontag he “had left such scant ground for hope.” But a brochure they are given to read about myelodysplastic syndrome infuriates him for its pussyfooting “refusal to write as if bad news were bad news and despair despair.” “In the end, what really seems unconscionable is the way in which the brochure is written in the language of hope, but in fact offers almost none to anyone reading it with care,” because of course this “disconnect” is fundamental to the reality, “the gap here between language and reality is simply too great and is actually a disservice to most patients….”
Sontag reacted to the news of her fatal illness with understandable grief and despair, but it didn’t stop her from learning all there was to know about myelodysplastic syndrome from medical texts and the Internet, and, most importantly, lining up a recognized expert in diagnosing and treating the almost always fatal disorder. Rieff, meanwhile, was going through what he calls “the loved one’s dilemma”:
The questions tumble out, in wakefulness and in dreams. At least, more than two years after her death, they continue to for me: Did I do the right thing? Could I have done more? Or proposed an alternative? Or been more supportive? Or forced the issue of death to the fore? Or concealed it better?
On the evidence of his book, Sontag understood and participated fully in her own case, yet he himself was largely excluded. By his account, Sontag was unresigned almost to her last breath to the death that people around her had accepted as probably inevitable from the time she was diagnosed with the last fatal blood condition. When she decided to fight, her only son, and many friends, could only support her, but now, with inevitable hindsight, Rieff asks himself what he could have done differently.
Rieff’s nuanced view of his famous mother is evident; he praises her astonishing determination to live, but mentions it so often that the rhetorical effect is to suggest something excessive in her, a bloom of narcissism or egotism beyond the usual, or at least a power of denial beyond the usual. Rieff is left to ask the tormenting question—did I do the right thing?—without seeming to know what that would be.
It is a question most survivors ask themselves, under a variety of circumstances, about the death of a family member, but it pertains finally to the psychic comfort of the asker more than to objective reality. He wonders if he should have told her the truth about her condition; he wonders if he should have fostered her state of denial of death. He wonders if they should have done something else, somehow saved her from the futile measures and painful end she herself wanted to try. It is a tormented conversation he is having with himself; the reader, in the position of eavesdropper, is free to draw different conclusions, perhaps, than Rieff himself does.
The Sontag he portrays had an unreserved will to live, and determination to do everything to save her own life, no matter how painful or how long the odds. This is what she did, and so the world, while regretting her death, cannot but feel that it was a death she understood, and the death she chose, with no reproaches due her son or bereaved friends. From the reader’s point of view and based on what Rieff tells us, the answer to his question, could he have done more, absolves him. His own inability to absolve himself, arising from his relationship to Sontag, whatever its details, is another matter: “In any case, our relationship was not one in which I would have been drawn to ask her about any of this.” The “unanswerable questions of a survivor” are of course, his central problem.
The form of grief and its duration inevitably reflect the form of a relationship, though this is not an aspect of David Rieff’s book one is invited to explore. Interestingly enough, the Kübler-Ross emotional sequence experienced by the dying is also said to be felt by the survivors of someone’s death, with the last stage, acceptance, when it finally comes, having the power to attenuate despair.
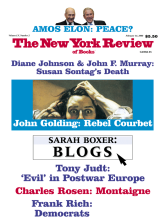
This Issue
February 14, 2008
-
1
Susan Sontag, Illness as Metaphor and AIDS and Its Metaphors (Anchor, 1990).
↩ -
2
Lucien Israël, Conquering Cancer, translated by Joan Pinkham (Random House, 1978).
↩ -
3
See Elizabeth A. Mittendorf, George E. Peoples, and S. Eva Singletary, “Breast Cancer Vaccines: Promise for the Future or Pipe Dream?” Cancer, Vol. 110, No. 11 (October 15, 2007), pp. 1677–1686.
↩ -
4
David K. Espey, Xiao-Cheng Wu, Judith Swan, et al., Annual Report to the Nation on the Status of Cancer, 1975–2004, Featuring Cancer in American Indians and Alaska Natives (American Cancer Society, National Cancer Institute, Centers for Disease Control and Prevention, and North American Association of Central Cancer Registries, published on line, October 15, 2007).
↩ -
5
Macmillan.
↩ -
6
“Illness as More Than Metaphor,” December 4, 2005.
↩