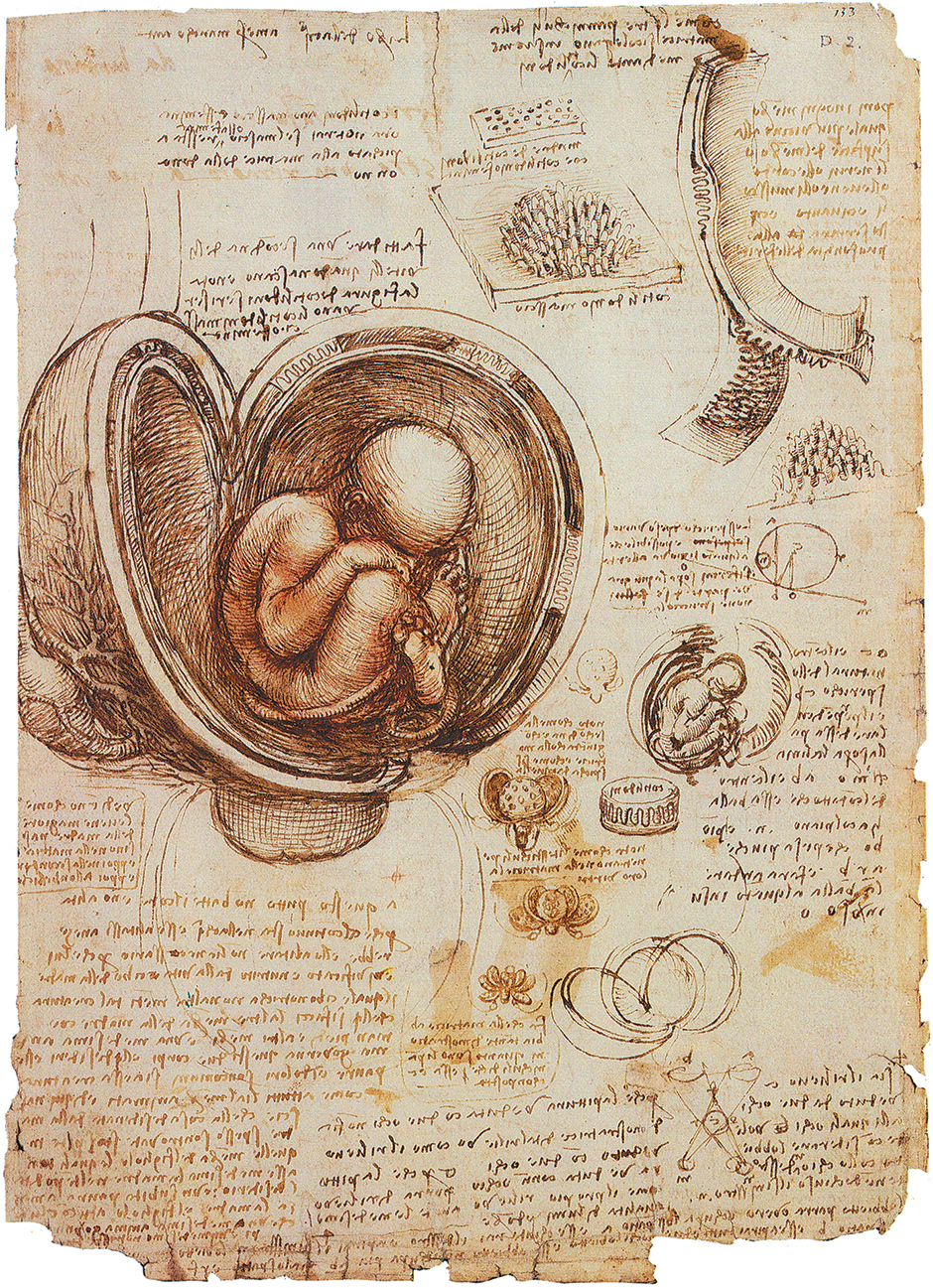
During the 1960s, with the introduction of the Pill, sex became separated from its reproductive consequences. In 1977, the British scientists Robert Edwards and Patrick Steptoe successfully carried out an in vitro fertilization (IVF), the process by which an egg is fertilized outside the body—ex utero—and the embryo is transferred into a woman’s uterus several days later.
These two advances—the Pill and IVF—very quickly changed the realities of human reproduction in a way that had been difficult to imagine only a few years before. In an insightful book, The XX Factor,1 Alison Wolf describes the way some of these changes in reproductive technology, particularly the Pill, have affected the lives of many well-educated and relatively affluent women: especially those who are now able to avoid unplanned pregnancies and who have successfully pursued careers in previously male-dominated professions.
Yet if they intend to have one or more children, many women are faced with a dilemma: the years during which women can conceive and carry a pregnancy to term are limited, and they coincide with some of the most important years in their professional lives. Of course many women in this position choose natural conception through intercourse during their early professional years. But it has now become clear that the use of IVF, in a recently developed form, could ease the dilemma of many fertile women, possibly bringing about changes as momentous as those brought by the Pill.
During the last fifty years, the average age of women in Europe at first childbirth has increased from twenty-five to thirty years. According to recent data in the UK, female university graduates now have their first child at thirty-five years. As women age, two factors are of primary importance in the decline in their fertility: the ovarian factor, concerning the supply of eggs in a woman’s ovaries, and the uterine factor, concerning the part of the body where the fertilized egg is to develop.
Problems with the uterus differ widely among women, and can often be helped with hormonal support therapy in conventional gynecological practice. Problems with the ovaries, on the other hand, affect most women in much the same way as they age. Women are born with their life’s supply of eggs, and at thirty-five years old, 95 percent of these eggs are gone. At this point, the remaining eggs are aging, which can cause complications when a child is conceived. Babies born to women beyond their late thirties are five times more likely, for instance, to have Down’s syndrome. These ovarian problems have been the subject of an extraordinarily rapid and extensive worldwide research effort.
One way of circumventing these problems would be for women in their twenties to freeze their young eggs. Then, when they decide they want children later in their careers, they will have the option to conceive using these eggs—which could be fertilized by the sperm of their partners at this later stage in their lives, or from a sperm bank. Previously, this had not been possible. Embryo cryopreservation—the preservation of a fertilized egg by freezing—had been widely used, especially by infertile couples trying to conceive using IVF fertilization. But only in the last few years has it become possible to freeze and thaw unfertilized eggs. These thawed eggs can then be fertilized by intracytoplasmic sperm injection (ICSI), a technique only invented in 1991, but which has since been used successfully in over one million cases. Using this technology, women can now realistically consider collecting and storing their young eggs for years, to be used at the desired later time by ICSI fertilization and transfer two to three days later of the embryo into her uterus, to have one or two children—the current norm in Europe and Japan.
The financial cost of these procedures is unlikely to be a barrier for the relatively well-to-do women who are most likely to make up the first group to use them. A major inconvenience for these women would be undertaking a hormonal drug-induced superovulation for one or two months in their early twenties, in order to release an adequate number of eggs for long-term storage. The effects that many women now experience when they undergo a superovulation should not be underestimated. Abdominal swelling, tension and pressure in the ovarian area, as well as mood swings are common; so is bruising from the many injections that are required during the process.2 This is not to mention the risk of less common but serious complications, such as Ovarian Hyperstimulation Syndrome (OHSS), which can be fatal.
Yet it should be noted that during the last few decades at least 20 million women have chosen some form of superovulation, most of them women whose fertility is impaired and who are pursuing IVF treatment, frequently without success. This impaired fertility explains why the number of attempted superovulations is much higher than the number of births through IVF, which currently stands at about five million.
Advertisement
For women to undergo a superovulation and to store their young eggs is, first of all, a kind of insurance. Women may still decide to conceive through sexual intercourse. There are, however, other advantages to storing and preserving eggs at an earlier age. It is now possible, for instance, to carry out genetic analyses on a single cell of an embryo that is fertilized outside the uterus before it is implanted in it. Such genetic analysis enables women to screen for certain birth defects and avoid using a defective embryo. For many fertile women who plan on having no more than one or two children, and are prepared to pay for such information, this would be a major incentive to pursue the IVF route to conception rather than ordinary coitus.
In my view, during the next few decades the number of women using this type of simplified IVF who do not have fertility problems will overtake those with impaired fertility. This is a crucial point that has been virtually ignored by critics of the wider use of noncoital methods of reproduction, who often cite possible post-delivery complications or low success rates. They do not take into account that most studies of currently used IVF focus on parents with impaired fertility. In the majority of cases, their subjects are also older women with older eggs.
This is very different from the situation I have outlined in which fertile women, using their stored young eggs, may choose ten or more years later to have children by means of embryo transfer into their uterus, with a success rate that may approach the success rate of fertilization through sexual intercourse.
It should not be ignored that fertile women who choose such embryo transfer may nevertheless encounter some of the side effects—some transient, some serious—of IVF as it is now practiced by fertility-impaired women. In addition to the side effects and risks of superovulation described above, these commonly include transitory mood swings, headaches, and taking many injections or pills for several weeks.
There is also a higher likelihood of complications among women pursuing IVF. These include pregnancy-induced hypertension3; pulmonary embolism (4.2 compared to 2.5 women out of 1,000)4; and pre-eclampsia—a disorder characterized by high blood pressure, the presence of protein in urine, and fluid retention, which can develop into a fatal condition without treatment—although recent research has questioned the likelihood that the latter can be caused by IVF alone.5 Such factors should enter into the personal calculations of risks and benefits by women considering IVF. These women should also remember, however, that normal coital reproduction at an advanced age carries its own risks.
Unless procedures can be revised and improved, as I feel sure they will be, a large number of women may not be willing to take these risks. (To suggest some of the problems, I have listed in the accompanying footnotes some articles that should be easily accessible to readers.)
At the same time, readers should be aware that women who do decide to delay childbirth until after the age of thirty-five also incur a confirmed series of risks. As a document distributed by the British National Health Service indicates, these include high blood pressure and risk of pre-eclampsia, as well as the risk of complications during pregnancy and delivery, such as prolonged labor.6 Women who undergo an embryo transfer late in their reproductive years may also face some of these risks, although they will not face the higher likelihood of Down’s syndrome.
If the number of fertile women who choose fertilization by IVF will ultimately be as high as I predict, the costs of IVF in many countries (though perhaps not in the US, where medical costs continue to escalate) will decrease dramatically, or they will be covered by health insurance, as is already the case in several countries. If this happens, many of those women are then also likely to choose concomitant sterilization as their method of birth control, as I predicted some fifteen years ago.7 (Apart from the changing factor of cost, some women may ask why concern themselves for years with contraception when the desired child will be created through noncoital methods?)
I should emphasize that I am making a prediction not about the immediate future but about the next couple of decades. An enormous amount of research is being conducted that almost certainly will improve the present conditions for superovulation and IVF. But even if there were no progress, we have no idea whether particular young women who save their eggs and are otherwise healthy and fertile will suffer from any or many of the problems cited.
Advertisement
A similar form of cryopreservation should also be considered by men. The freezing and storage of sperm is already successfully practiced in sperm banks, where the sperm of donors is stored for use in treatments of couples whose fertility is impaired. This procedure requires a single act of masturbation and so is much simpler and cheaper than the cryopreservation of the eggs in ovarian tissue.
Moreover, recent studies in Iceland and in Sweden have offered persuasive evidence that the children of older fathers are more subject to some risks—for example mental disorders—than the children of younger fathers.8 We can expect, then, that just as women will make increasing use of stored eggs for IVF reproduction, some men will start using stored younger sperm to avoid such risks and to protect their future children.
This Issue
September 25, 2014
The Cult of Jeff Koons
Obama & the Coming Election
Failure in Gaza
-
1
Crown, 2013; reviewed in these pages by Marcia Angell, “The Women at the Top,” March 20, 2014. ↩
-
2
“The Medical Procedure of Egg Donation,” web.stanford.edu/class/siw198q/websites/eggdonor/procedures.html. ↩
-
3
Martin Beckford, “Women Who Have IVF at Higher Risk of Complications,” The Telegraph, October 20, 2011. ↩
-
4
Peter Henriksson et al., “The Incidence of Pulmonary and Venous Thromboembolism in Pregnancies After in Vitro Fertilisation: Cross Sectional Study,” BMJ, January 15, 2013. ↩
-
5
Noriyoshi Watanabe et al., “Is In Vitro Fertilization Associated with Preeclampsia? A Propensity Score Matched Study,” BMC Pregnancy and Childbirth, Vol. 14, No. 69 (2014). ↩
-
6
“Warning to Older Mothers,” British National Health Service, June 2009. ↩
-
7
Carl Djerassi, An Immaculate Misconception: Sex in an Age of Mechanical Reproduction (London: Imperial College Press, 2000). ↩
-
8
Brian M. D’Onofrio et al., JAMA Psychiatry, Vol. 71, No. 4 (2014), a conclusion that The New York Times of February 26, 2014, headlined as “Mental Illness Risk Higher for Children of Older Fathers, Study Finds.” ↩