London—“There are plenty of things people will say we got wrong,” Britain’s prime minister, Boris Johnson, said of the nation’s coronavirus response in a recent speech. In one of the world’s worst affected countries, much of the focus has been on government mismanagement. Johnson’s inexperienced cabinet, selected for fealty to Brexit over anything else, has proved inept and out of its depth. With the Downing Street inner circle dominated by hardliners of the Vote Leave campaign, the response to the crisis was botched and negligently slow—the Brexit preoccupation diverting resources from pandemic planning. Before even any official inquiry is under way, many regard Johnson himself as ultimately responsible: quoted in a damning investigation by the UK’s Sunday Times newspaper in April, a senior adviser to the government condemned the prime minister’s fecklessness: “He didn’t do urgent crisis planning. It was exactly like people feared he would be.”
Britain’s official toll of Covid-19 deaths has passed 44,000. Going into lockdown late may have cost thousands of lives. Releasing potentially infected hospital patients into elderly care homes exposed the most vulnerable to risk—more than one in twenty of nursing home residents are believed to have died from Covid-19, a figure roughly thirteen times higher than for the same population in Germany. But the serial mismanagement of the crisis, as disastrous as it’s been, conceals a deeper failing, one driven by ideology.
Boris Johnson won last year’s December election on promises of Brexit, but also state investment and “leveling up” neglected regions of the country. And yet, facing the coronavirus crisis, his party’s instinct was to shore up the private sector: a pandemic version of “disaster capitalism,” to borrow Naomi Klein’s coining from her 2007 book The Shock Doctrine. Britain’s public health sector, a cash-strapped, eroded, but functioning network comprising the National Health Service (NHS), general-practice clinics, and local authority health officials, has been repeatedly sidelined in favor of outsourced alternatives. As Allyson Pollock, a professor of public health at Newcastle University, put it to The New York Times recently: “They’re basically trying to build a centralized, parallel, privatized system.”
This happened even as scientists and health experts urged government to use the existing, practiced, and more effective public sector. It happened while UK media reports from countries that got a better grip on the coronavirus crisis, from Germany to the Indian state of Kerala, showed the vital part played by public health care. I spoke to Dr. Tony O’Sullivan, the co-chair of the campaign group Keep Our NHS Public, who said the pandemic has been exploited as an opportunity “for those who have been trying to return healthcare to the private sector, a long-standing project.” Putting Covid-19 contracts in private hands undermined Britain’s coronavirus response at the beginning of the pandemic and leaves it still lurching today.
*
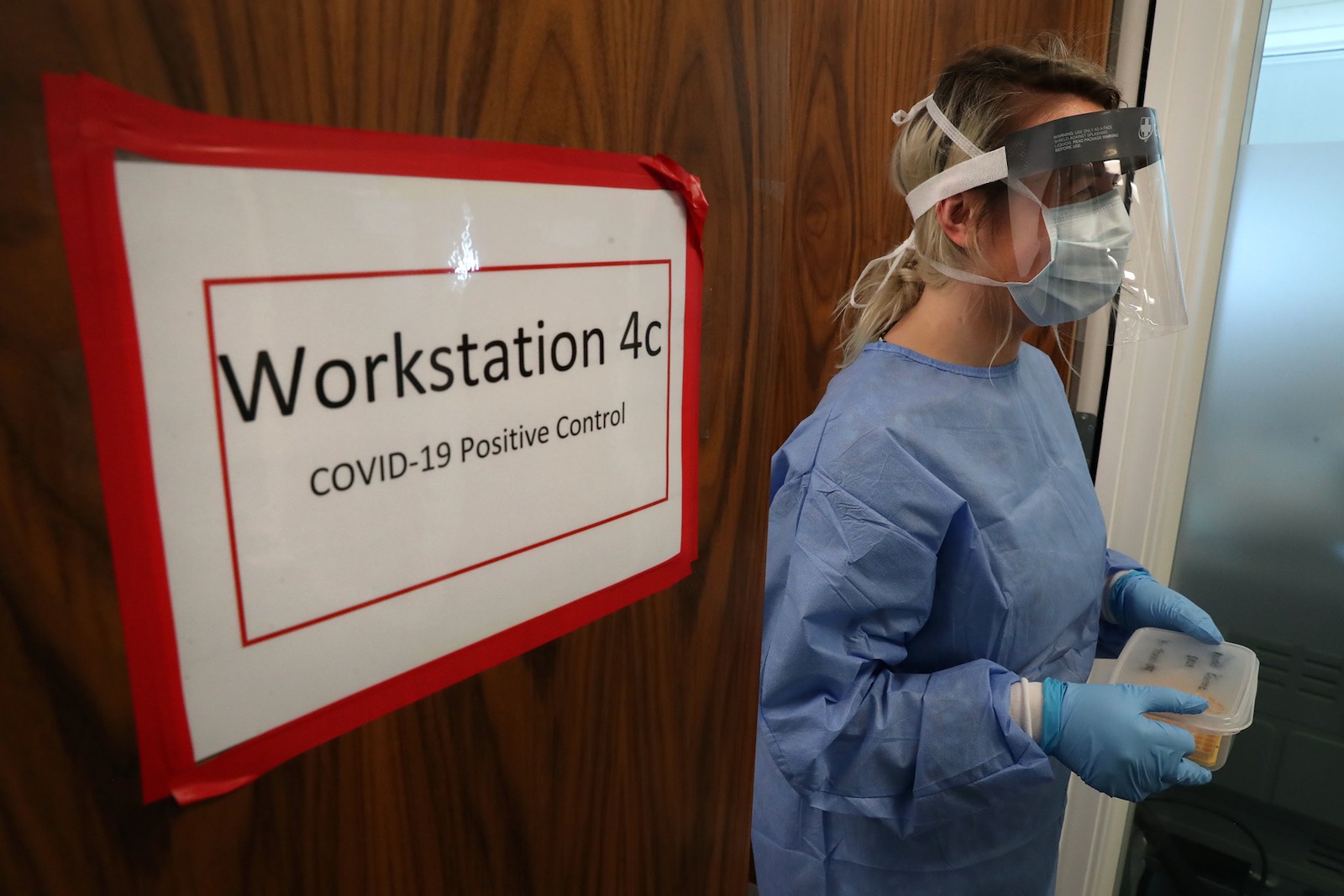
Before the end of May, more than three hundred NHS and nursing home workers had died from Covid-19, along with many transport and other essential workers. Dr. Abdul Mabud Chowdhury, an East London-based doctor who died from Covid-19 in April at the age of fifty-three, had warned about the lack of personal protective equipment (PPE) five days before being hospitalized; by then, it was clear that Britain was struggling to provide these crucial supplies. The government, tardy in stockpiling, blamed “global shortages” as countries raced to meet demand. But Britain’s response was also hamstrung by decades of fragmentation and outsourcing, and a decade of punishing austerity cuts that hit local government and public services hard. We Own It, a group that campaigns for social ownership for public services, reports that even prior to the coronavirus, NHS supply chains had been sliced into eleven procurement areas dealing with various private contractors. Convoluted and often reliant on just-in-time practices, this supply chain fell down in the face of the pandemic.
In late March, trying to address PPE shortages, the government brought in the Army and also contracted with the retail distributor Clipper Logistics, whose chief executive, Steve Parkin, is an ardent Conservative who cites former Tory leader Margaret Thatcher as a hero and has donated £725,000 ($900,000) to the party in the past five years. Through April, there were reports that this system was still floundering and local authorities were having to make their own arrangements to equip NHS and care workers. The accountancy firm Deloitte was brought in to source equipment through a crisis unit under the direction of the Cabinet Office in Whitehall. According to manufacturers, this initiative proved to be a “disaster.” One factory owner told The Daily Telegraph: “It has been a nightmare to deal with Deloitte,” since the firm did not understand how supply chains worked.
Advertisement
Day after day, the government said it was open to all offers of help to make protective wear. Some eight thousand PPE suppliers duly emailed the cabinet office, but many never received anything more than an automated reply. Hiring Deloitte for the job was an error of judgment, according to a manufacturer, one of those offering to help, who spoke to the UK political website OpenDemocracy: “If there is a fire, you don’t call the auditor, you call the fire service.” The site reports that several manufacturers spoke of the sleep loss and anxiety caused by knowing they could have done something to help, if only they had been asked to.
Early in the pandemic, the WHO chief, Dr. Tedros Adhanom Ghebreyesus, had said, “Our key message is: test, test, test”—but Britain did not heed this advice. In mid-March, the official criteria for testing, through the NHS, extended only to hospitalized cases of infection and essential workers. The government failed to activate the full network of laboratories at its disposal—within the NHS, as well as in universities and independent research facilities. When the government did finally roll out wider testing, months later, it again bypassed existing labs and set up three, new mega-facilities whose operations—managed by Deloitte under the banner of “lighthouse laboratories”—have been based on contracting arrangements about which there’s little public disclosure.
The Francis Crick Institute, a nonprofit biomedical lab, was one of many facilities to offer help. It swiftly created and published testing protocols, which were downloaded thousands of times. The institute can run up to 5,000 daily tests, with fast turnaround, but the government has shown little interest in its offer of help. “We were not taken seriously, or any notice of,” said Paul Nurse, the institute’s director. Offers from labs like his around the country “could have made a significant difference at the height of the pandemic,” he told me. The Institute of Biomedical Science, a body that represents some 130 NHS labs has also criticized the government’s decision to ignore the existing system for providing testing. “It just seems perverse that we created this whole additional structure rather than looking at what was in their own backyard,” its president, Allan Wilson, told HuffPost, adding that it was hard not to see “an element of political dogma” at work.
Unveiled amid much fanfare in early April, the mega-labs ran into trouble within weeks. Privately contracted drive-through centers set up to take swabs for testing were hard to access and did not always produce usable samples. At one point, as many as 350,000 samples could not readily be matched to records because the drive-through centers had not logged people’s NHS IDs; and of some 67,000 samples that were sent to the US for testing in early May, nearly 30,000 came back void. Reviewing this testing program, the Royal College of Pathologists has cited a damning list of failures: “poor specimen taking, poor labelling or poor transcription of details, slow result turnaround, poor quality control, lack of the result being returned to the appropriate person, inappropriate application of the result, and lack of clinical input or oversight.”
The logistics of sending swabs to faraway labs and the results back to local authorities or hospitals itself creates margins of error of the sort that might be avoided through an existing public system where local government, the NHS, and doctors’ surgeries are already connected. Sarah Calkin, deputy editor of Local Government Chronicle, told me of the “huge frustration” among senior officers. “Councils had leisure centers closed, libraries, and other venues already existing in their communities where people could have gone to get testing,” instead of the remote drive-throughs set up for the purpose. Directors of public health within local authorities say they were not consulted. “It was all done in a black box in central London,” as one put it to me.
All of this meant that local authorities could not determine infection rates in their own districts, often finding out about outbreaks in their areas first from local media. When the complete, local level data first started to appear, it showed councils had previously seen only the tip of the iceberg of infections. “We spent the first part of the pandemic to well past the peak flying blind, with only half of the confirmed cases visible in the public domain,” said Dominic Harrison, director of public health in Blackburn, in northwest England.
This issue recently made national news after an outbreak of infections in Leicester forced the East Midlands city into a local lockdown. Leicester’s mayor and public health officials said they had not received pillar 2 testing for their area, which meant that 90 percent of recent cases were detected by local facilities and were not counted in national data. Like other local authorities, this council did not until recently have postcode-level data on infections, which is essential for controlling outbreaks.
Advertisement
But testing was only half of the problem: government mismanagement also hindered efforts to use this information to track the virus and limit its spread across the population. A fledgling, minimal tracing operation that involved calling contacts of those found to be infected and ordering them to self-isolate was halted in mid-March, amid much criticism. Then, in early May, the government announced it was setting up contact-tracing call centers that would be staffed by thousands and would work alongside a new tracking app. It was touted by government ministers as a “world-beating” system—hyperbolic rhetoric that drew a response from opposition leader Keir Starmer that “effective will do.” In the event, the system has not even cleared this bar.
The low-paid staff of call-center companies Serco and Sitel who responded to recruitment ads calling for a “positive can-do attitude” and a “passion for customer services” have described chaotic training, unwieldy tech systems, and idle shifts for lack of Covid-contact calls to make. Serco’s appointment, in particular, raised eyebrows—both because the company was recently fined more than £1 million ($1.25 million) for failures on another government contract and because junior health minister Edward Argar is a former lobbyist for the company. Originally scheduled to be up and running in June, the track-and-trace system will not now be fully operational until September. In a leaked email, Serco’s chief executive said he wanted the scheme to “cement the position of the private sector” in the NHS supply chain.
Meanwhile, the government’s much-vaunted, custom-built tracing app flunked—after three months of wasted development time and at a cost of several million pounds. It has been abandoned in favor of existing technology from other developers, though it is not clear when this version will be integrated into the government’s track-and-trace program either.
According to the British Medical Journal, by late June local health protection teams had traced nearly eight times more contacts than the outsourced call centers and online services had. Local authority expertise was obvious to anyone who knows anything about public health, Chris Ham told me. The former chief executive of an independent healthcare think tank, the Kings Fund, is now the chair of the Coventry and Warwickshire Health and Care Partnership Board, a nonprofit that coordinates local government and health services in the Midlands. “It is what they are trained to do, bread and butter to them,” he said. “It’s about knowing your community, the sociology, the anthropology of different areas. It cannot be done nationally by people in call centers.”
Central government has now brought local authorities partly into to the process and given them extra funds, but until this point, Ham said: “Councils were banging on government doors saying, ‘Use us, we want to play our part, we know what to do.’” In a recent online press conference for a group of experts and scientists known as Independent Sage, Gabriel Scally, a former regional director of public health, said that a failure to make better use of public health and local resources would have significant economic consequences, as the UK would likely now “bump along with a continuing infection, with hotpots and flare-ups, maybe even a second wave.” Instead of “investing in a proper and effective system,” the Johnson government’s policy choices would “create much more damage.”
Nobody knows the overall price tag for outsourcing. Though some £1.7 billion ($2.1 billion) in private-sector contracts has been disclosed, full details are not public. Ian Makgill, director of OpenOpps, a group that monitors public-sector contracts, has said: “There seems to be a feeling in government that ‘we can get away without publishing information.’” Some clues come from Professor Pollock and colleagues, who have noted that the annual budget for communicable disease control for Public Health England, an arm of the health department that is leading the government’s coronavirus response, was £87 million ($109 million) in 2018–2019; by way of contrast, Randox Laboratories won a month-long contract for analyzing home-testing kits worth more than £133 million ($167 million) alone.
“It is about political will,” she said, at a recent event held by Independent SAGE, a group of independent scientists that aims to provide transparent advice on the coronavirus outbreak. “It is squandering hundreds of millions [of pounds] on contracts that are not going out for tender.” The Conservative member of Parliament Owen Patterson is currently paid £100,000 ($125,000) a year as a consultant for Randox, which won the contract unopposed. As Labour member Tan Dhesi reminded Parliament in mid-June, the government had suspended normal procurement rules and a competitive bidding process during the pandemic. “Lo and behold,” he said, “major Tory party donors and prominent members on the government benches—including ministers, may I add—have major shareholdings or are inextricably linked to many of these firms.” Talking to me, he described the slew of private-sector pandemic contracts as purely “ideological.” In this case, it’s not even “privatization through the back door,” he said—the pillaging is taking place in full view.
*
There is a larger game afoot in all this. The outsourcing bonanza has coincided with Britain’s tense talks with the European Union over the terms of a new, non-member relationship. The Brexit transition period, during which Britain is still following EU rules, concludes at the end of the year. Negotiations to resolve myriad difficult, outstanding issues have already been set back by the pandemic, yet Boris Johnson has refused to countenance an extension. For Vote Leave hardliners, a no-deal Brexit is not unwelcome: it would, as they see it, set the nation free to forge ahead as Global Britain, a sort of deregulated “Singapore-on-Thames,” as some Brexiteers have enthused.
Others see this as a dangerous new “shock doctrine” (Klein’s phrase again). Parting ways with his increasingly “hard Brexit” party last year, the former Conservative chancellor Phillip Hammond wrote in The Times of London that Johnson’s advisers “see the shock of a disruptive no-deal Brexit as a chance to reorder our economy and society.” Coupled with rolling back the welfare state through a handout of pandemic contracts to the private sector, this bonfire of regulations represents an extension of Thatcherism, a chance to finish what she started.
Although Johnson himself is opportunistically ambivalent and won the last election in part on promises of lavish public spending in favor of Britain’s “left-behinds,” this harder-edged political ethos runs through his administration. Even short of Britain’s crashing out of the EU in a hard Brexit, a bare-minimum trade deal with its former European partners would leave the UK seeking to deepen trade relations with other countries—especially the US, where disdain for freedom-crushing “big government” and red tape is an inspiration for many in the now-ascendant right of Johnson’s Conservative Party. But if the ideological appeal to Downing Street of an American deal is clear, the cost for practically everyone else will be considerable.
“Modern trade deals are about so much more than tariffs,” Nick Dearden, director of the campaign group Global Justice Now, told me. “They are about regulation, how you run public services, what kind of food standards you have.” For the US, a trade deal is contingent on opening up British markets in food, farming, pharma, and health services and that will means battering down the existing standards and protections that came with EU membership. With those lowered standards, the UK would not be able to carry on trading in the EU market. The Conservative manifesto for last December’s election promised not to compromise on Britain’s food, animal welfare, and environmental standards. But Johnson’s government has since backtracked on those commitments, refusing to guarantee that chlorinated chicken from the US would stay off UK shelves, and refusing to amend a recently passed agriculture bill to include greater protections for British farmers.
There is scant public support for any of this: in recent polling, the vast majority of Britons are unwilling to accept lower-quality US imports. But since the Conservatives have an eighty-seat majority in Parliament—and since the government last year scrapped powers for parliamentarians to scrutinize post-Brexit trade deals—there is no legislative mechanism to scrutinize or stop any trade deal.
The country is now headed for a post-pandemic recession, which, the Organization for Economic Cooperation and Development forecasts, is likely to be one of the worst among the major economies. According to pro-Brexit analysts recently cited by The New York Times, the government could bury the shock of Brexit, which may entail a no-deal default to WTO terms, in the generalized pain of the pandemic. But as one Scottish National Party member gloomily predicted in Parliament in early June: “It’s going to be misery heaped on misery as Covid and Brexit appear like the twin horsemen of the economic apocalypse, trampling over any prospect of a recovery.”