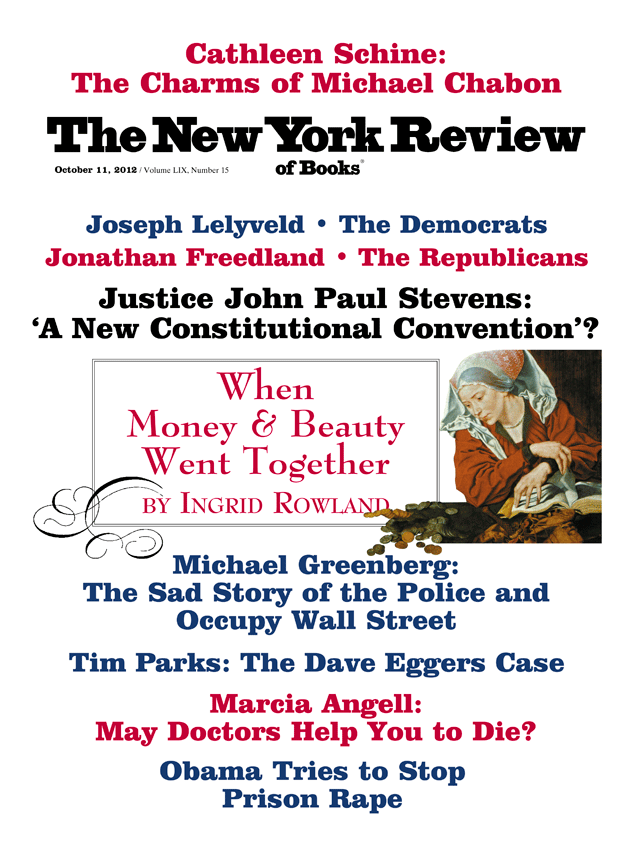
On November 6, Massachusetts voters will decide whether a physician may provide a dying patient with medication to bring about a faster, easier death if the patient chooses. On the ballot will be a Death with Dignity Act that reads:
It is hereby declared that the public welfare requires a defined and safeguarded process by which an adult Massachusetts resident who has the capacity to make health care decisions and who has been determined by his or her attending and consulting physicians to be suffering from a terminal disease that will cause death within six months may obtain medication that the patient may self administer to end his or her life in a humane and dignified manner. It is further declared that the public welfare requires that such a process be entirely voluntary on the part of all participants, including the patient, his or her physicians, and any other health care provider or facility providing services or care to the patient.
If this ballot initiative passes, it will be binding, and Massachusetts will join Oregon, which implemented a virtually identical statute in 1998, and Washington, which did the same in 2009, as the only states where voters approved this form of physician-assisted dying, sometimes called aid-in-dying. (These terms are favored by proponents over the older term, physician-assisted suicide, because they distinguish it from the typical suicide in which someone with a normal life expectancy chooses death over life. Here the patient is near death from natural causes anyway, and chooses the timing and manner of an inevitable death.) Montana, through a 2009 decision by its Supreme Court, not a voter referendum, also permits physician-assisted dying.
Euthanasia—the act of directly injecting medication to cause death rather than providing medication for the patient to take if he or she chooses—is also a form of assisted dying, but it is banned everywhere in the United States. It is also banned in Switzerland, where assisted dying is otherwise allowed. However, euthanasia is legal in the Netherlands, Belgium, and Luxembourg, where they make no moral distinction between the two forms of assisted dying, and euthanasia is favored because it’s easier and faster. In June, the British Columbia Supreme Court overturned the Canadian law against assisted dying.1 If that decision stands on appeal, Canada will likely join the Benelux countries in allowing both forms of assisted dying.
The growing number of jurisdictions permitting physician-assisted dying, and particularly its possible acceptance in heavily Catholic Massachusetts, might suggest a new movement, but in fact what we are seeing is an outgrowth of a decades-long evolution in public attitudes toward how we die, which began with the 1976 case of Karen Ann Quinlan. Quinlan was a young woman found unconscious and not breathing after taking Valium and drinking heavily at a party. Although she was resuscitated, her brain was irreversibly damaged, and she was kept alive in a permanently unconscious state with a mechanical ventilator and a feeding tube. After several months, her parents decided to disconnect the ventilator and allow her to die. But they were required to get legal permission, and the case eventually reached the New Jersey Supreme Court.
In a landmark decision, the court authorized Quinlan’s father, who had been appointed her legal guardian, to stop all life-sustaining treatment if he so chose.2 (Unexpectedly, she continued to live even after the ventilator was removed, and since her parents were unwilling to stop artificial feeding, she lived, unconscious, for another nine years.) As the Quinlan case unfolded, it received extensive media coverage, and people began to say that they “wouldn’t want to live like Karen Ann Quinlan.”
Before Quinlan, there wasn’t much explicit attention given to whether and how to bring about an earlier death in permanently unconscious patients, or in patients who, although conscious, were suffering unbearably at the end of life. In fact, in the 1960s, when I trained in medicine, dying was hardly mentioned in medical school or training programs, except as a failure of treatment. It was rarely spoken of to families, let alone patients, who were never to be denied hope for a recovery, no matter how dire the prognosis. Sometimes when patients were in obvious misery at the end of life, doctors would increase the dose of morphine, with the expectation that it would hasten death, but they usually didn’t consult with anyone about it (an order for a large dose of morphine could lead to trouble even in those days), and it was more a reflection of doctors’ compassion and courage than patients’ needs and desires.
There were a few, isolated concessions to the inevitability of death during this period. In 1957, Pope Pius XII held that there is no moral requirement for doctors or families to provide “extraordinary” medical treatment, by which he seemed to mean futile or extremely burdensome treatment.3 In 1968, a group of prominent physicians recommended that death be redefined to include brain death even while respiration and heartbeat continued, and that treatment could be withdrawn from such patients.4 Also in the 1960s, Dame Cicely Saunders introduced the British hospice movement to the United States, and Elisabeth Kübler-Ross published her book, On Death and Dying, which argued for greater acceptance of death. Nevertheless, until the case of Karen Ann Quinlan, removing life-sustaining treatment, particularly artificial feeding, would generally have been considered tantamount to euthanasia, and simply was not done.
Advertisement
Nor was it nearly as urgent a question as it later became. Before the time of Quinlan, we simply didn’t have the technology to sustain life artificially for very long. In addition, there was another reason the right-to-die movement began about the time of Quinlan. As medicine became more specialized, of necessity it became a team endeavor, not a purely private matter between one physician and one patient. So a physician could not quietly increase the dose of morphine, as before. Instead, these sorts of decisions were removed from the bedside, discussed among team members, and became subject to ethical and legal oversight.
Within six months of the Quinlan decision, California became the first state to pass a Natural Death Act, which gave physicians legal immunity, with some restrictions, if they complied with patients’ directives in “living wills” to withhold certain life-sustaining treatments. One after the other, the remaining states passed their own versions of the Natural Death Act. In 1990, the US Congress enacted the Patient Self-Determination Act, which required all hospitals that receive federal funds (and that’s nearly all of them) to inform patients of their rights to prepare advance directives, to refuse treatment for any reason, and to name a proxy to act for them if they lost the capacity to make such decisions.
Also in 1990, the US Supreme Court addressed the issue in the case of Nancy Cruzan, a young woman in a condition much like Quinlan’s (termed a persistent vegetative state), whose parents sought to have her feeding tube removed. Although the Supreme Court denied their request because Cruzan had not left “clear and convincing evidence” that this is what she would have wanted, as required by her home state of Missouri, the Court did hold that if she had left such evidence, or in states where there was no such requirement, artificial feeding or any other life-sustaining treatment could be stopped.5 (Later, friends obligingly presented such evidence, and she was allowed to die.)
Much of the ethical underpinning for the wave of legislation and legal decisions that followed the Quinlan case was provided by the President’s Commission for the Study of Ethical Problems in Medicine in its influential 1983 report, “Deciding to Forego Life-Sustaining Treatment.” In it, the commission argued that not only was it ethical to forgo life-sustaining treatment, but there was no moral distinction between withholding and withdrawing it, and no distinction between artificial feeding and other life-sustaining treatment.6
Earlier, it had been considered more of a problem to withdraw treatment than not to start it in the first place, and artificial feeding was given special status. By the end of the 1980s, then, just fourteen short years after the Quinlan decision, it had become well established that patients could refuse any form of treatment, either directly or through an advance directive or proxy. (Unfortunately, experience since then has shown that advance directives are honored mainly in the breach; a 1995 survey found that most are disregarded by physicians, who may not even be aware that they exist.)
So far, I’ve focused on the refusal of treatment, not assisted dying. But the right to refuse life-sustaining treatment presupposes that there is such a treatment to refuse. Suppose there isn’t. Many dying patients might not be receiving such treatment because they can live without it. For example, although some patients with widespread lung cancer might need a mechanical ventilator to survive, patients with widespread cancer of the pancreas, which can also inflict terrible suffering, might not need that or any other treatment to remain alive while they slowly die in great misery. Shouldn’t they have the same right to hasten their deaths? In 1980, Derek Humphry founded the Hemlock Society, which not only argued for legalizing assisted dying, but published information on how to end one’s life if there was no treatment to withdraw. Still, the assisted dying movement did not enter the mainstream of public debate in the US for another decade, and was generally shunned by the medical establishment.
It wasn’t until 1990 that the issue began to have traction, and that was largely because of the emergence of two very different proponents—essentially a “bad cop” and a “good cop”—whose actions captured widespread public attention. The bad cop was Dr. Jack Kevorkian, a Michigan pathologist who set out on a nationwide crusade to help people end their lives with contraptions he devised that would allow them to trip the injection of a lethal substance or the inhalation of carbon monoxide. These people had disparate ailments, some of them terminal, some not, and Kevorkian had no long-term relationship with them or any clinical input from relevant specialists. Many in the medical profession were horrified, but surprisingly, much of the public approved of what he was doing. Although the Michigan legislature enacted a law against assisted suicide mainly to stop Kevorkian, and he was prosecuted four times under it, juries refused to convict him. It was not until he had performed euthanasia on television, that is, directly killed a patient, after nine years of assisting in some 130 suicides (according to his lawyer), that he was convicted of second-degree murder and sent to prison.
Advertisement
The good cop was Dr. Timothy Quill, an internist in Rochester, New York, who in 1991 published in the New England Journal of Medicine a moving account of his decision to help a patient end her life.7 His patient, whom he called Diane, was a forty-five-year-old woman with leukemia. Without a bone marrow transplantation, which would entail much discomfort and was unlikely to be successful, she would die. Diane decided to refuse the transplantation and, with the support of her husband and adult son, asked Quill for a prescription to bring about death if and when she chose. He agreed, gave her the prescription, and she ultimately ended her life by taking it, after first asking her family to leave the house for an hour or so. Quill, who had been Diane’s physician for eight years, concluded his account by asking “why Diane, who gave so much to so many of us, had to be alone for the last hour of her life.”
At the time, I was executive editor of the New England Journal of Medicine and was aware that if we published Quill’s article, he might be at some legal risk. Like thirty-five other states, New York had banned assisted suicide. When I phoned Quill to ask whether, in light of the risk, he wanted to reconsider his request to publish the account of Diane’s death, he took a few days to think about it, then said he wanted to go ahead. Almost immediately after publication, the county district attorney brought him before a grand jury to indict him for manslaughter, but the grand jury refused.
In contrast to Kevorkian, Quill became widely respected within the medical profession, partly because his thoughtfulness was so at odds with Kevorkian’s indiscriminate zealotry. He became an influential spokesman for assisted dying as a last option in caring for terminally ill patients, and did much to bring it out of the shadows. He also became the plaintiff in a lawsuit to overturn New York’s prohibition against assisted dying.
That lawsuit wended its way toward the US Supreme Court, along with a similar one that originated in Washington State. In both cases, the relevant appeals courts (the 2nd Circuit, which has jurisdiction in New York, and the 9th Circuit in Washington) held that laws forbidding physician-assisted dying were unconstitutional. Both based their decisions on the liberties protected by the Constitution’s Fourteenth Amendment, which would include the right to determine the manner of one’s death. Finally, in 1997, the US Supreme Court, in Vacco v. Quill and Washington v. Glucksberg, reversed the appeals courts, declining to find a federal constitutional right to assisted dying, although reserving the possibility that it might do so in the future and making it clear that death hastened by palliative measures was permissible. Crucially, the Court held that for the moment the question of allowing assisted dying should be left to the states.8
Meanwhile, in 1994, to almost everyone’s surprise, following defeats of ballot measures in Washington and California, Oregon voters narrowly approved a Death with Dignity Act—the first law of its kind anywhere in the world.9 An effort to repeal the law three years later failed by a 60–40 majority, and assisted dying under the law began in 1998. Two organizations were instrumental in this achievement. One, formed by Portland attorney Eli Stuts- man, who drafted the act and shepherded it through its early years, has evolved into the Death with Dignity National Center (its state chapter led the Massachusetts effort). The other, Compassion & Choices, the outgrowth of several mergers and name changes (a progenitor was the unfortunately named Hemlock Society), had earlier sponsored the first Death with Dignity initiative in Washington State, which although it failed provided valuable lessons for Oregon. Largely through the efforts of its indefatigable director of legal affairs, Kathryn Tucker, Compassion & Choices was also crucial in successfully defending the Oregon law from various legal challenges, culminating in a 2006 victory in the US Supreme Court.10
Oregon’s law has a host of safeguards—in fact, some believe too many. First, it applies only to adults who are able to make their own decisions at the time of the request. It cannot be used through advance directives, or by people with limited decision-making capacity. Second, the patient must have a terminal illness, with a life expectancy of no more than six months, as determined by at least two physicians. That means it excludes patients who are suffering from an irreversible medical condition, such as amyotrophic lateral sclerosis (“Lou Gehrig’s Disease”), but are not within six months of death. (The Benelux countries, Switzerland, and British Columbia would not exclude such patients.)
In addition, the patient must make two oral requests for medication to hasten death, separated by at least fifteen days, and one written request, with two witnesses. By definition, the patient must be capable of swallowing the medication—usually barbiturates dissolved in a full glass of liquid—which ensures that it is voluntary. The law does not permit euthanasia. If the physicians believe a psychiatric condition is impairing the patient’s judgment, they must refer him or her to a psychiatrist or other counselor. No physician is required to participate in assisted dying; they may refuse for any reason whatsoever.
The Oregon Health Authority’s Division of Public Health keeps detailed records of how and why the law is used, which it releases every year.11 The law has now been in effect for nearly fifteen years, and it seems to have worked pretty much exactly as intended. As of the end of 2011, it had been used to hasten death by 596 patients, accounting for only one in five hundred deaths in Oregon. Most had cancer that had metastasized, although some had other terminal illnesses, such as advanced emphysema, and nearly all were receiving hospice care. Over 94 percent of the deaths occurred at home. The main reason patients gave for wanting to hasten their death was the loss of autonomy. Although pain was given as a reason by about a fifth of patients, it was near the bottom of the list. Roughly a third of all patients who were prescribed the medication did not take it, but kept it at hand because it provided peace of mind.
Concerns about an ethical “slippery slope” have not been borne out. First, the great majority of requests in Oregon were denied (in 1999, about 80 percent). Although there has been an increase in the incidence of assisted dying over the years, from sixteen deaths in 1998 to seventy-one in 2011, that was to be expected as people became more familiar with the law. It is still used sparingly, and the point of it, after all, was to make assisted dying available. At first, there were fears that the availability of physician-assisted dying might crowd out good palliative care, but it has had the opposite effect. Most experts believe that Oregon now has among the best palliative care in the country. There were also concerns that the law would be used disproportionately by disadvantaged patients—for example, the poor and uninsured. But in fact, the patients who died in Oregon were relatively affluent and well educated, and almost all had health insurance. They were the type of people who particularly value control and independence. Furthermore, there has been no indication of coercion by unscrupulous family members.
Whether patients who requested assisted dying did so because they were depressed is more difficult to evaluate.12 The symptoms of depression overlap with those of terminal illness, and dying inevitably produces sadness. Moreover, there are no good studies of the effectiveness of therapy in this setting. So far, the limited evidence is that depression is no more frequent in the patients who request assisted dying than in other terminally ill patients. Nevertheless, the Death with Dignity laws, including the ballot initiative in Massachusetts, require physicians to refer patients for counseling if they believe a patient’s judgment is impaired by depression or another psychiatric condition, and that was a common reason Oregon doctors gave for denying requests for assisted dying.
In short, observers looking for a slide down a slippery slope have not found it. No law, of course, works absolutely perfectly, but this one seems to come about as close as possible. It is overwhelmingly supported by the public and, according to one study, by most physicians in Oregon. The experience in Washington, although shorter, is much the same.
All of these laws exclude euthanasia. The rationale is that if the patient must swallow the medication, it is a voluntary act, whereas euthanasia could be involuntary. Many doctors gloss over that distinction, because they believe both forms of assisted dying are unethical in that they require the active participation of doctors in ending life. Even some doctors who believe assisted dying is sometimes warranted say they would not write the prescription themselves, but would outsource it to someone else.
These doctors, however, do not usually object to withdrawing life-sustaining treatment, such as a mechanical ventilator, if requested by a patient or proxy, because they don’t see it as actively causing death. Aside from the fact that disconnecting a ventilator would appear very active, indeed would constitute homicide, if done without the consent of the patient or a proxy, the problem with this argument is that it puts the focus on the physician, not the patient. If looked at from the patient’s point of view, swallowing medication is a purposeful action the patient must take, unlike withdrawing treatment or euthanasia, in which the patient may be passive.
Organized medicine is all over the map on this issue. The American Medical Association opposes physician-assisted dying altogether, stating in its Code of Ethics that it “is fundamentally incompatible with the physician’s role as healer.” But the American Medical Association now represents no more than 30 percent of physicians, and other medical organizations, such as the American Medical Students Association, the American Public Health Association, and the American Medical Women’s Association, support assisted dying. The Massachusetts Medical Society House of Delegates, knowing of the ballot initiative, strongly reaffirmed its opposition to assisted dying last December.
I have long favored legalizing physician-assisted dying for terminally ill patients whose suffering cannot be relieved in any other way, and I was the first of the original fourteen petitioners to put the Massachusetts Death with Dignity Act on the ballot in November. In 1997, as executive editor of the New England Journal of Medicine, when the issue was before the US Supreme Court, I wrote an editorial favoring it, and told the story of my father, who shot himself rather than endure a protracted death from metastatic cancer of the prostate.13
It seems to me that, as with opposition based on whether the physician is “active,” the argument that physicians should be only “healers” focuses too much on the physician, and not enough on the patient. When healing is no longer possible, when death is imminent and patients find their suffering unbearable, then the physician’s role should shift from healing to relieving suffering in accord with the patient’s wishes. Still, no physician should have to comply with a request to assist a terminally ill patient to die, just as no patient should be coerced into making such a request. It must be a choice for both patient and physician.
Probably most dying patients, even when suffering greatly, would choose to live as long as possible. That courage and grace should be protected and honored, and we should put every effort into alleviating their symptoms. But not all suffering can be adequately relieved. Most pain can be eased, but other symptoms are harder to deal with—weakness, loss of control of bodily functions, shortness of breath, and nausea—and the drugs to treat those symptoms often produce side effects that are as debilitating as the problems they treat. Even worse for many dying patients is the existential suffering. They know their condition will worsen day by day until their deaths, that their course is inexorably downhill, and they find it meaningless to soldier on. Why should anyone—the state, the medical profession, or anyone else—presume to tell someone else how much suffering they must endure as their life is ending?
As the November election draws near, the Massachusetts battle over assisted dying will become hard fought, and it is not at all clear which side will win. The Catholic Church is adamantly opposed, and Cardinal Seán O’Malley, the archbishop of Boston, has referred to assisted dying not as compassionate, but as an act of “sheer brutality.” But Catholics don’t necessarily follow the teachings of the Church’s hierarchy; for example, most Catholic women use some form of artificial birth control, despite the Church’s opposition. A 2005 Harris poll found that 70 percent of adults favor assisted dying, but when Americans have had the chance to vote for it, they sometimes pull back, as they did most recently in Maine in 2000. The tide appears to be turning, however. Nearly everyone knows someone who has died a slow, difficult death, and there is a natural desire to try to give patients more control over how they die. If the Death with Dignity Act is approved in Massachusetts, it will be a major step in that direction.
-
1
Carter v. Canada (Attorney General), 2012 BCSC 886, June 15, 2012. ↩
-
2
In re Quinlan, 70 N.J. 10, 355 A.2d 647 (1976). ↩
-
3
Pius XII, “The Prolongation of Life,” The Pope Speaks, November 24, 1957. ↩
-
4
“A Definition of Reversible Coma: Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death,” The Journal of the American Medical Association, August 5, 1968. ↩
-
5
Cruzan v. Director, Missouri Department of Health, 497 U.S. 261, 110 S.Ct. 2841 (1990). ↩
-
6
President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research, “Deciding to Forego Life-sustaining Treatment: A Report on the Ethical, Medical, and Legal Issues in Treatment Decisions” (Government Printing Office, 1983). An early and important analysis of end-of-life issues by a group of distinguished experts in medicine, law, and bioethics. ↩
-
7
T.E. Quill, “Death and Dignity—A Case of Individualized Decision Making,” The New England Journal of Medicine, 324 (1991). ↩
-
8
See Kathryn E. Tucker’s comprehensive article on the legal challenges to assisted dying, including the Supreme Court’s decision in Vacco v. Quill and Washington v. Glucksberg, “Legal Advocacy to Improved Care and Expand Options at the End of Life,” in Physician-Assisted Dying: The Case for Palliative Care & Patient Choice, edited by T.E. Quill and M.P. Battin (Johns Hopkins University Press, 2004). ↩
-
9
See Eli D. Stutsman’s authoritative account of the history and implementation of the Oregon Law, “Political Strategy and Legal Change,” Physician-Assisted Dying: The Case for Palliative Care & Patient Choice, edited by T.E. Quill and M.P. Battin (Johns Hopkins University Press, 2004). ↩
-
10
Gonzales v. Oregon, 546 US 243 (2006). ↩
-
11
See the Division of Public Health’s easily accessible year-by-year and overall results. ↩
-
12
Dr. Ganzini, a psychiatrist, has carried out some of the most difficult research on attitudes in Oregon toward assisted dying, and has tried to evaluate the influence of depression; see “The Oregon Experience,” Physician-Assisted Dying: The Case for Palliative Care & Patient Choice, edited by T.E. Quill and M.P. Battin (Johns Hopkins University Press, 2004). ↩
-
13
Marcia Angell, “The Supreme Court and Physician-Assisted Suicide—The Ultimate Right,” The New England Journal of Medicine, January 2, 1997. See also “The Quality of Mercy,” Physician-Assisted Dying: The Case for Palliative Care & Patient Choice, edited by T.E. Quill and M.P. Battin (Johns Hopkins University Press, 2004). Here I recount attitudes toward dying before Quinlan, and also tell the story of my father in more detail. ↩