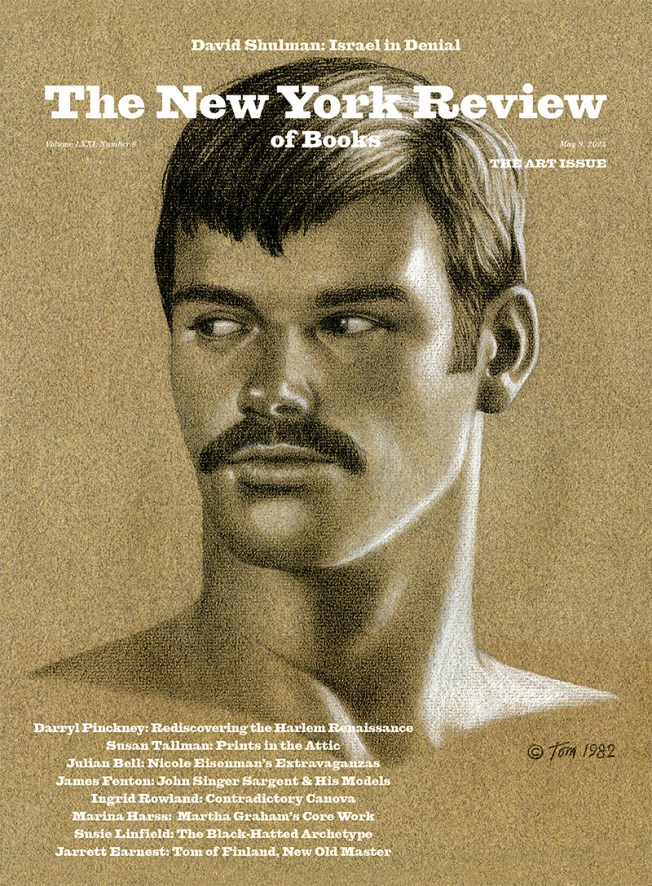
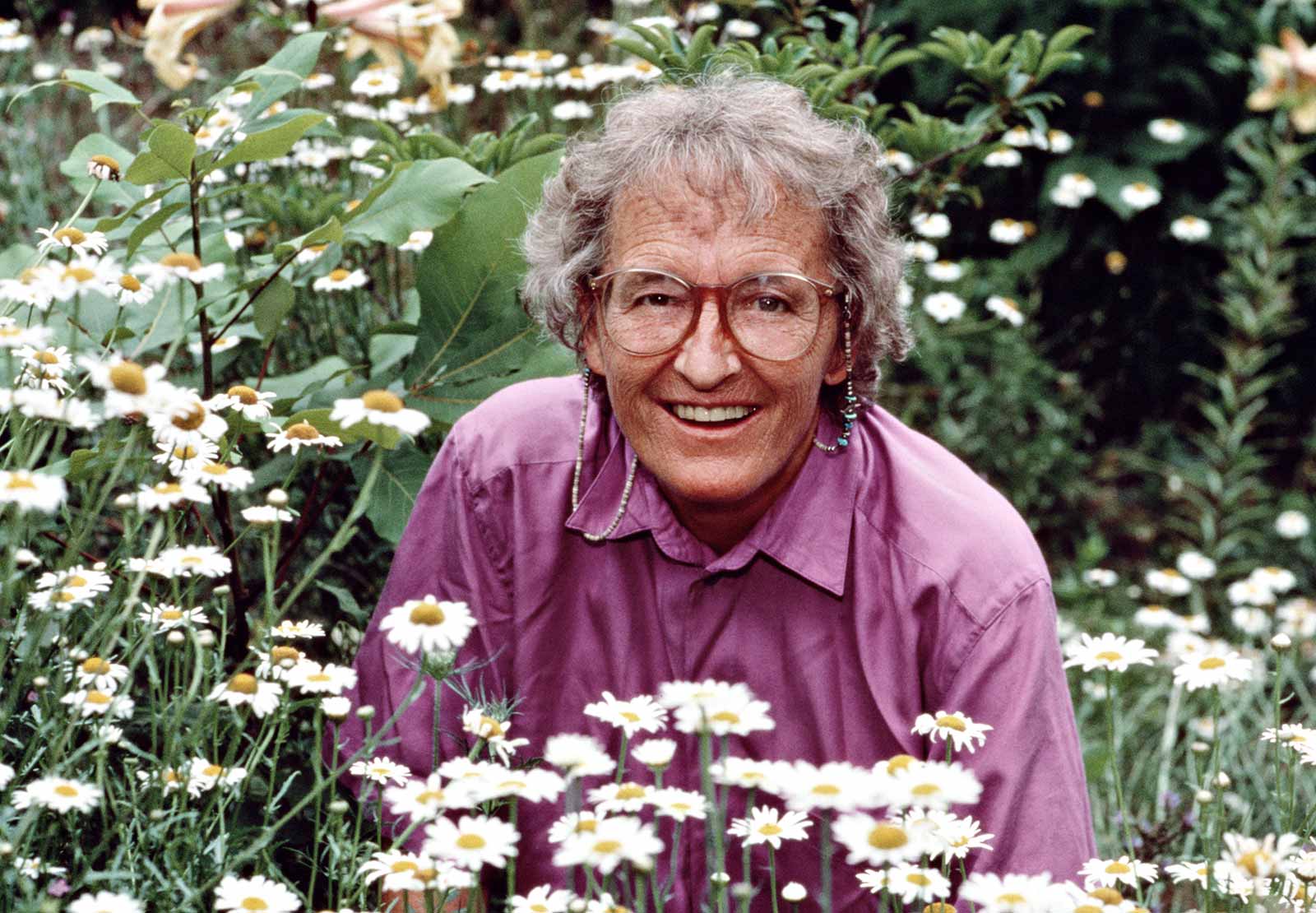
So much about death is unknowable: Cancer or car accident? What happens next? But when Elisabeth Kübler-Ross was thirty-seven years old, she decided that she was going to learn everything there was to know about it. There was no precedent for this course of study. At the time, she was a professor and doctor at the hospital affiliated with University of Chicago, and she began conducting interviews with terminally ill patients. The interviews were open-ended, lasting as long or as short as the patient wanted. The patients talked about their pain, their loneliness, their frustrations with their medical care. They talked about the irksome parts of illness, like urinating into a catheter, and their fear of endless blackness.
“You still want to be a person,” said a young nun with late-stage Hodgkin’s disease. “All the kind people who pushed the wheelchair just drove me to distraction because they pushed me to where they wanted me to go, not where I wanted to go.” Another patient, a middle-aged woman with leukemia, sensed that her doctors were withholding information from her. “They have not told me what they found during the operation,” she said. “Why in the world can’t they talk to me? Why can’t they tell you before they do certain procedures? Why don’t they let you go to the bathroom before they take you out of the room, like a thing, not like a person?”
Kübler-Ross collected these interviews in her book On Death and Dying: What the Dying Have to Teach Doctors, Nurses, Clergy and Their Own Families, which was published in 1969. The book bears the rigorous obsession of a scientist on the brink of discovery. She is long-winded and detailed, as interested in the forest as she is in the trees. After thousands of hours of interviews, she reached the conclusion that the process of dying could be loosely broken into five stages—denial, anger, bargaining, depression, and acceptance. Kübler-Ross later said that she never conceived of the stages as linear or all-encompassing, that the main lesson from the two and a half years she spent interviewing terminally ill patients was that they desired to be treated as individuals with complicated and layered feelings rather than as patients with a fixed set of medical needs. “It’s not a map,” said David Kessler, who was a frequent collaborator of Kübler-Ross. “No two people are going to go through the stages exactly alike.”
Kübler-Ross later applied the same five stages to the process of grieving. And, as with dying, she never meant to imply that grief was contained to just five feelings, or that the stages were linear, like levels in a Nintendo game. “They were never meant to tuck messy emotions into neat packages. They are responses to loss that many people have, but there is not a typical response to loss, as there is no typical loss. Our grief is as individual as our lives,” she wrote in On Grief and Grieving, which she co-wrote with Kessler (and was published a year after her death in 2004).
Over the years, as the stages have disseminated across popular culture, readers have interpreted Kübler-Ross’s stages as complete and successive, a conclusion that reflects less what was written than a desire among caregivers and doctors for a concrete process to guide them beyond the brink of uncertainty. The original book, as stated in its subtitle, wasn’t intended as medical textbook but as a project that would inspire more empathy for the dying. “It is simply an account of a new and challenging opportunity to refocus on the patient as a human being, to learn from him the strengths and weaknesses of our hospital management,” she wrote.
Her relationship with these patients continued long after she published the book and well past their deaths. The people she interviewed reappeared months and years after their funerals, visiting her at work and at home. She’d see them in the elevator after lectures, apparitions that spoke to her with the clarity of a pilot warning about oncoming turbulence. They even left little notes on her desk. She became interested in life after death, and though she never claimed to have studied the afterlife, she claimed to understand it all the same. In the later years of her career, she wrote about the afterlife with the confidence of an anthropologist who had returned from fieldwork. “As soon as your soul leaves the body, you will immediately realize that you can perceive everything happening at the place of the dying,” she wrote in On Life After Death, published in 1991. “You do not register these events with your earthly consciousness, but rather with a new awareness.” Friends and colleagues worried about her, that bearing witness to so much despair had frayed her mind and loosened her grip on reality.
Advertisement
Kübler-Ross heard these rumors. “Many people say: ‘Of course Doctor Ross has seen too many dying patients. Now she starts getting a bit funny,’” she wrote. She insisted that she was fine, better than fine. She was known among friends as the most upbeat, energetic person in the world. Though she was a doctor by training, “at home in laboratories,” as she’d written in her journal, she was liberated by the possibilities of nonscientific inquiry. To understand the afterlife, she relied on simulations with psychedelic drugs, consultations with mediums, and loose thought experiments. There was more than one way to be an expert, Kübler-Ross seemed to argue: you could study, or you could simply know.
*
Kübler-Ross’s memoir, The Wheel of Life, reads like a fairy tale. Its villains are cruel and ogre-like, weakened by arrogance; hardships always end in victory; fates are written at birth. “I was destined to work with dying patients,” she writes. She comes across, from the beginning, as an inspiring but unreliable narrator.
She was born in Zurich, the first of triplets, and weighed two pounds. The doctor, who considered herself a clairvoyant, looked down at the three babies and predicted that the youngest child, who was six pounds and healthy, would be her mother’s favorite; the middle child, who was also born precariously underweight, would “choose a path in the middle.” When she looked down at Elisabeth, she said, “You will never have to worry about this one.”
And so begins Kübler-Ross’s journey, one of a restless, curious woman seeking truth despite the well-meaning men who stand in her way. At six, a teacher asked her to write an essay about what she intended to be when she grew up. When she told her parents about the assignment at dinner that night, her father, a middle manager at an office-supply company, told her that she should plan for a career as his secretary. “No, thank you!” young Elisabeth snapped. That night, she wrote in her journal that she planned to become a physician and an adventurer. “I want to find out the purpose of life.”
When she graduated from high school, she moved out of the house and found a job as an apprentice in a chemical lab. A few years later, in 1945, she joined the International Voluntary Service for Peace, a European organization that served as the model for the Peace Corps, and traveled to France, Poland, and Germany rebuilding war-torn villages, handing out food, restoring schoolhouses, and providing basic medical care. She realized then that healing had more to do with compassion than medicine. “The best thing we gave those people was love and hope,” she wrote.
When she returned to Zurich, she borrowed money from her sister and enrolled in a local medical school, where she met Emanuel Ross, an American who had fought in the war and was paying for school through the GI Bill. They married in 1958 and moved to Long Island, where they both found internships at a hospital.
In Long Island, she developed a taste for chewing gum, hamburgers, and sugary cereals. She began to wear pants more often than skirts. But she was appalled by certain social aspects of American culture. At the hospital, she found the doctors indifferent, the children rude, and their mothers complete pushovers. “One day in the children’s ward I watched a spoiled brat throw a colossal fit when his mother forgot to bring a toy,” she wrote. “What were these American mothers and their children thinking? Didn’t they have any values? What good was all that stuff when what a sick child really needed was a parent to hold his hand and talk openly and honestly about life?”
In 1959, she was offered an internship in the psychiatric unit at Manhattan State Hospital, where she tended to forty schizophrenic women. They were guinea pigs, she wrote in her memoir, enrolled in an experiment to test the efficacy of new medications and LSD. Her job was to administer these experiments and complete the research logs, but instead, she taught the women independent living skills. They learned to comb their hair, dress themselves, and arrive to appointments on time. She took them on field trips and helped them find jobs and their own apartments.
Her program was so successful that she was interviewed for a job running the pharmacological unit at Montefiore, a private hospital. During her interview, the director of Montefiore, whom she describes as having the “personality of a cold fish,” tried to show off, asking about her experience treating addicts and neurotics, but only so he could expound on his own expertise. She was not impressed. “Knowledge helps, but knowledge alone is not going to help anybody,” she recalled telling him. “If you do not use your head and your heart and your soul, you are not going to help a single human being.”
Advertisement
He hired her despite this outburst. But after a few years, she and Manny decided it was time to leave New York. They moved to Colorado for bit, and in 1965, they moved to Chicago along with their two children, Kenneth and Barbara. Manny took a position at Northwestern University in the neuropathology department while she completed a PhD in psychology and joined the psychiatric department at the University of Chicago, where she met her fate—introduced, as it often is in fairy tales, by an unexpected knock on the door.
She was in her office at the University of Chicago when four seminary students paid her a visit. They were researching death and dying: they wanted to know how to best serve congregants who had ill loved ones or were ill themselves. They asked if she’d be willing to serve as a liaison between the seminary and the hospital, to coordinate interviews with terminally ill patients. They’d heard that she’d written a paper on the psychology of dying. She hadn’t, but she took their mistake as a sign.
Every Monday, she arranged a seminar where a dying patient spoke about his or her experiences to a room of rapt seminary students. The patient spoke before a one-way mirror, with the students observing from the other side. She’d ask the dying patient about how they were feeling and their relationships with their doctors. “Patients weren’t shy about expressing their dissatisfaction with their medical care—not the actual physical care, but the lack of compassion, empathy, and understanding,” she wrote.
Medical students were invited to attend the seminars, but for a long time, none did. “The physicians have been the most reluctant in joining us in this work,” Kübler-Ross noted in On Death and Dying. “It may take both courage and humility to sit in a seminar which is attended not only by the nurses, students, and social workers with whom they usually work, but in which they are also exposed to the possibility of hearing a frank opinion about the role they play in the reality or fantasy of their patients.”
American doctors were so preoccupied with avoiding death that they avoided any discussion of it. “I observed the desperate need of the hospital staff to deny the existence of terminally ill patients on their ward.” This was typical for the medical profession at the time. In the early 1970s, years after Kübler-Ross began her research, only about 10 percent of doctors told their patients when they had a terminal condition; until 1980, the American Medical Association considered it a doctor’s right not to tell their patients if they had an incurable disease. At Kübler-Ross’s hospital, most doctors would inform the patient’s family of a fatal diagnosis and allow them to decide what to share with the patient.
According to Peter Stearns, a professor and historian of emotions, Americans were demonstrative mourners during the decades after the Civil War, when the bereaved were presumed to be inconsolable. But by the mid-twentieth century, Americans had begun to encourage stoicism in the wake of a loss, with writers describing the painlessness of death and instructing mourners that the only way to survive grief was to ignore it. In the 1930s, the American Mercury, a popular magazine, carried the foreboding headline “America Conquers Death” and boasted that “death, which dominates European’s thoughts, has been put in its proper place in America.” A 1950s etiquette writer named Amy Vanderbilt instructed mourners to keep their feelings to themselves. “We are developing a more positive social attitude towards others, who might find it difficult to function well in the company of an outwardly mourning person,” she wrote.
Dorothy Dix, Ann Landers, and Dear Abby were a bit more empathic, offering their condolences and acknowledging the necessity of tears, but they also advised mourners to seek out distractions. When a father wrote to Dix about losing his seven-year-old son in a car accident, she recommended that he adopt a young child in need. A widow once wrote to Dear Abby comparing her loneliness “to a cancer, but worse” and Abby suggested that she seek out volunteer work. “There are lonely people to visit, blind folks to read and write for,” she wrote. They nudged their readers out of the house; they saw no purpose in wallowing.
Many of Kübler-Ross’s peers at the hospital considered her seminars exploitative and ghoulish and believed it cruel to force sick patients to ruminate on their own deaths. Kübler-Ross, in turn, felt that doctors were failing their patients and behaving irrationally. “I think modern medicine has become like a prophet offering a life free of pain. It is nonsense,” she wrote. “Medicine has its limits, a fact not taught in medical school.”
“When we look back in time and study old cultures and people, we are impressed that death has always been distasteful to man and will probably always be,” Kübler-Ross wrote in On Death and Dying. “Man has basically not changed. Death is still a fearful, frightening happening and the fear of death is a universal fear even when we think we have mastered it on many levels.” She empathized with doctors who had deep thanatological dread but was disheartened that they were unable to override their fears for the sake of their patients.
*
Doctors loved Kübler-Ross’s five stages. The stages gave doctors the capacity to diagnose their dying patients, to target their questions and categorize the evidence: if the patient wasn’t depressed, then maybe she was in denial. The stages provided guidance on what to say in impossible circumstances. She had, unwittingly, provided doctors with a system for discussing death like a medical process. Her collaborator, Kessler, told me that on more than one occasion, a medical colleague would stop by while he and Kübler-Ross were writing to seek help with a diagnosis. “They’d be like, ‘Elisabeth, what stage are they in?’ And she would say, ‘It’s not about the stages! It’s about meeting them where they are!’” She found it laughable how some doctors had the gall to hold an essential organ in their hand but had no capacity for ambiguity.
Friends say Kübler-Ross had a certain genius for meeting people where they were. Here’s one story her son, Ken Ross, told me: She was interviewing a patient whose mouth was wired shut, whose speech was limited to grunts. None of the other doctors or nurses could understand her, only Kübler-Ross. When the interview was complete, she instructed a wide-eyed physician to bring up an apple from the cafeteria. He pointed out that the patient wouldn’t be able to eat it and Kübler-Ross ignored him. She had left the patient’s hospital room by the time he returned, apple in hand. The patient broke into tears. The doctor brought her paper and pen so she could explain. She wrote that she’d spent her life as a teacher and had told Kübler-Ross that she missed receiving apples from her students.
Kübler-Ross loved doing the interviews, but they exhausted her. She had to cut herself off after four hours. She was not an impartial observer of the dying. She was convinced that people close to death accessed a frequency of consciousness and a capacity for kindness that no one else could. “What you learn from dying patients, you can pass on to your children and to your neighbors,” she wrote. She believed that there was no such thing as a premature death, that people died as soon as they’d learned everything they needed to know, and that her dying patients were closer to enlightenment than anyone else she knew. “For me, death is a graduation,” she liked to say.
Kübler-Ross believed that every dying patient passed through all five stages but could repeat a phase or experience two or more at the same time. Even denial and acceptance, two directly opposing ideas, could occur simultaneously. “Even the most accepting, the most realistic patients left the possibility open for some cure,” she wrote in On Death and Dying. There were other feelings, like guilt and regret, that weren’t stages, exactly, but companions throughout the process. She wrote of patients who felt guilty for burdening their family members or leaving children behind, and who regretted the years wasted away at work or in front of the television, as if there were no such thing as time.
*
In 1972, at the age of forty-two, Kübler-Ross lost her patience altogether with clinical settings. She was frustrated by the way her research had been misinterpreted by her medical colleagues and decided to devote herself full-time to her traveling seminar, “Life, Death, and Transition.” It was a weeklong series that included an eclectic mix of exercises “geared towards helping people overcome the tears and anger in their lives.” The workshops, which she held everywhere from California to Indiana, involved silent prayers and ritual fires where participants discarded their unwanted feelings and participated in exercises designed to release anger by punching a mattress or snapping a short rubber hose. There were assigned periods for wailing and screaming—she’d found that “active expulsion” of one’s feelings was more effective than talking. “Sometimes it pays not to think with your head as much as with your instinct,” she wrote.
She was on the road more often than she was at home. Her son Ken told me that she’d come home on weekends, cook meals and dessert for the entire week, and leave again. He was a teenager at the time, and he’d sometimes tag along to a weekend conference so he could see his mom. Her name was on the covers of People and Playboy, and she became the kind of celebrity who was sometimes stopped by strangers on the street.
Also in 1972, Kübler-Ross testified before the Senate’s Special Committee on Aging in a hearing called “Death with Dignity.” It had been seven years since President Lyndon Johnson created Medicare, a government program that subsidizes the health-care costs for the elderly, and in that time, government spending on nursing home care had more than doubled. “Medicare puts entirely too much emphasis upon institutionalization of patients, thereby increasing costs of treatment and anxiety among patients,” explained Senator Frank Church, a Democrat from Idaho and a member of the aging committee, in his opening statement. They were seeking humane and affordable alternatives to hospitalization.
“We live in a very particular death-denying society,” Kübler-Ross told the senators. “We isolate both the dying and the old, and it serves a purpose. They are reminders of our own mortality.” She made two recommendations. The first was to train medical students to care for the dying, to make the needs of the elderly and terminally ill as fundamental to medical education as cell biology or anatomy. As it stood, care for the dying fell to nurses, who were underpaid, overworked, and underprepared. (Kübler-Ross also advocated that these nurses have their hours reduced; the work, she said, was too exhausting to sustain eight to ten hours a day.) The second was to develop outpatient programs for the terminally ill, so that patients could spend their last days at home among loved ones. There was already a hospital in London that provided such services, which she pointed to as a potential model.
Two years after the hearing, a nursing professor at Yale, along with two doctors and a chaplain, founded America’s first hospice program in Branford, Connecticut. It had no physical facility; all of its doctors and nurses were dispatched to care for their terminally ill patients at home, as Kübler-Ross recommended. Hospice programs have proliferated in the decades since; there are now more than four thousand across the United States.
*
In the 1990s, Kübler-Ross experienced a series of strokes. She couldn’t walk or feed herself; she spent her last years sitting on the porch of her son’s Arizona ranch, staring out at the endless sky. She had visitors from all over the world. One woman flew in from Japan just for the day so she could have tea with Kübler-Ross before she died. When she was admitted to the hospital, a group of Native Americans in traditional garb showed up on Ken’s lawn, built a teepee, and smoked a pipe. There was a constant parade of journalists, who all wanted to know the same thing: How was the world’s expert on death responding to the loss of her own life? The answer: not well. She was crotchety, tired, and largely immobile, in a world of endless pain. She was “angrier than angry,” she told CNN. The journalist described Kübler-Ross’s response to dying as “very human.” Her reaction, the journalist wrote, was “not fully what I expected from the woman who created the model for coping well with death and dying.”
“People love my stages,” Kübler-Ross told Kessler shortly after the article came out and not long before she died, at the age of seventy-eight. “They just didn’t want me to be in one of them.”
This essay has been adapted from Asking for a Friend: Three Centuries of Advice on Life, Love, Money and Other Burning Questions from a Nation Obsessed published by Nation Books.