One of the main corporate participants in Operation Warp Speed, the Trump administration’s multibillion-dollar crash program to create and produce a Covid-19 vaccine, was Moderna. The federal government gave Moderna, which in 2019 was a small, unprofitable pharmaceutical firm, some $2.48 billion for vaccine development and bought millions of doses at $26 each for essentially free distribution to US residents. Moderna’s profits soared to $21 billion over the course of the pandemic. In late 2022, when federal subsidies seemed on the verge of ending, the company announced that it would soon offer an updated version of its vaccine at as much as $130 per dose. Many Americans were outraged.
Moderna’s behavior will not surprise readers of the journalist Alexander Zaitchik’s Owning the Sun, an indictment of American drug companies and the federal government for all too often privileging profits over health, and of the research universities, medical professionals, and philanthropists who have been deeply complicit with them. Ranging for the most part from the early years of the United States to the Covid-19 pandemic, the book shows how the drug industry and its affiliates operated in a state of ethical grace through much of the nineteenth century and in the twentieth fell from it with accelerating speed.
Zaitchik relies heavily upon recent studies that have called the prescription drug industry and its allies to account, for example Paul Farmer’s Pathologies of Power: Health, Human Rights, and the New War on the Poor (2003) and Graham Dutfield’s That High Design of Purest Gold: A Critical History of the Pharmaceutical Industry, 1880–2020 (2020). What distinguishes Owning the Sun is its aim to be a “people’s history” that tells the interrelated stories of drug commerce and the patent system “from the perspective of the dissenters, critics, and antagonists.” In his treatment of monopoly medicine Zaitchik at times slips into mere muckraking, offers simplistic interpretations, and stumbles into errors. His book is largely inattentive to the process of scientific invention and to the types of licensing rights that bring new products into use. It is also sloppily referenced.
Yet for all its flaws, Owning the Sun is an arresting provocation. Since World War II the pharmaceutical industry, aided by the federal government and philanthropic foundations, has produced an enormous arsenal of drugs against a variety of fearful diseases and disorders, but Zaitchik persuasively argues that it has also single-mindedly pursued profit maximization by engaging in price gouging, blocking the availability of cheaper generics, and exploiting the patent and regulatory systems to harass and suppress competition.1
In 1793 Congress updated what qualified for a patent: “any new and useful art, machine, manufacture or composition of matter, or any new and useful improvement [thereof].” (Except for the substitution of “process” for “art,” the definition of patent eligibility today remains essentially the same.) In keeping with British precedent, Congress limited exclusive rights to fourteen years. Most European nations allowed patents on the processes used to produce medications, but they had long associated medical knowledge with God’s blessings and held that it should be freely available, not under monopoly control.
While the United States did not prohibit patents on drugs, most of the “patented medicines” sold by entrepreneur apothecaries were not actually patented; that would have required the disclosure of ingredients that fabricators preferred to keep secret. In 1847 the founders of what became the American Medical Association (AMA) adopted a code of ethics that declared it “inconsistent with beneficence and professional liberality” to patent a medicine or prescribe a medicine that was patented. After the Civil War the pioneers of the American drug industry—rapidly growing firms such as the Squibb Corporation, Eli Lilly & Co., and Parke, Davis & Co.—aligned themselves with this code. These “ethical” firms also refrained from branding or trademarking their products. Trademarks, which have the potential for infinite renewal, could, Zaitchik writes, glossing the view of the Parke-Davis physician Francis Stewart, turn the “temporary monopoly [of a patent] into a permanent one by cementing the association between a brand and the medicine for all time.”
In the late nineteenth century, however, trends in both science and the market prompted drug companies to abandon this high ground. Scientists and physicians, many based in academia, were expanding the knowledge of disease, and drug companies were opening their own research laboratories to devise novel medications. To protect these drugs from competitors, they began patenting not only their processes but also the drugs themselves. Stewart contended that this practice was consistent with the ethical obligation to circulate medical knowledge: “A thing patented was a thing divulged.”
The industry’s embrace of patents was encouraged by formidable competition from abroad, notably Germany, where synthetic dyestuff firms were applying their expertise in organic chemistry to the invention of effective pharmaceuticals. Zaitchik spotlights the Bayer Company, which introduced three remarkable pain relievers, one of them aspirin, to the American market at exceptionally high prices. Despite an outcry by consumers and their allies, the drugs, effective as well as nonaddictive, were bought by the millions.
Advertisement
The increasing availability of patented drugs transformed them from suspicious promotions by patent medicine quacks to reputable products of laboratories. They became commonplace during World War I, when the federal government seized German property held in the US, including patents and trademarks that it licensed to American firms, allowing for domestic production of some two hundred drugs that had previously been imported. The AMA, including its academic members, had also come around to patents after the Pure Food and Drug Act of 1906 prohibited the manufacture or sale in interstate commerce of adulterated or misbranded, including inaccurately described, foods and medications. Between the wars, Zaitchik writes, academic and corporate laboratories partnered to develop and test drugs, forging new codes of conduct around patenting that aimed to reconcile industry’s profit-minded practices with academic medicine’s long-standing ethical commitments. Their advocates insisted that, while professors should not profit from their inventions, patents allowed universities and other nonprofits to reserve their products for public benefit, as well as use them for income to support research.
By the early 1920s several universities had begun to pursue that model. Harry Steenbock, an agricultural chemist at the University of Wisconsin, discovered in 1923 that exposure to sunlight enhanced the amount of vitamin D in organic materials. Aware of a recent finding that a deficiency of the vitamin causes rickets, Steenbock expected that enriching foods and supplements with it would constitute a potent defense against the disease. Revenues from licenses on the patent, administered by the Wisconsin Alumni Research Foundation (WARF), inspired a number of other leading universities to follow suit, especially after the onset of the Depression.
Zaitchik dwells on how patents could compromise academia’s putative ethical standards. Sensitive to the interests of Wisconsin’s dairy industry, a powerful influence on state appropriations for the university’s agricultural work, WARF refused to license the vitamin D patent to producers of margarine, which was cheaper than butter and might have protected children of lower-income families from rickets. Yet to the editor of the state’s leading dairy journal, it seemed
that information discovered by the use of public money belongs to the public and it is difficult for me to understand how such discoveries can be patented and some private corporation determine how they shall be used.
Zaitchik is alive to the editor’s point in his excursions—brief for developments before World War II, extensive for those after it—into the history of the federal government’s patronage of science and the shaping of patent policy by the drug industry, Congress, and the courts. He draws on a report of the Temporary National Economic Committee, created by Congress in the late 1930s at the initiative of President Franklin Roosevelt, which held that corporations had come to use patents to achieve concentration of economic power and that it was now a task of government to reverse that trend. According to Zaitchik, that New Deal approach shaped the development of penicillin, the antibiotic discovered in Britain at the end of the 1920s and mass-produced during World War II. Central to penicillin’s production was a fermentation process devised by scientists at the Department of Agriculture and used under federal contracts by several major drug companies. Vannevar Bush, the head of the wartime scientific mobilization, saw to it that no company was allowed controlling rights to the drug.
But penicillin was an anomaly. During the war, some 90 percent of government research contracts granted contractors whatever patents might arise from their work, which the government then had a royalty-free license to use. Senator Harley Kilgore, a leader of the wartime initiative that led to the establishment of the National Science Foundation (NSF) in 1950, contested this convention; a liberal Democrat from West Virginia, he thought the government should hold the patents on any research it funded. Bush relentlessly resisted Kilgore on this point, arguing that contractors bring their own assets to the research, including laboratory facilities, technical knowledge, and the expertise to turn the knowledge to practical use.
The NSF’s bylaws, Zaitchik writes, ultimately included “a ‘loose’ patent regime that allowed agency chiefs to determine patent policy on a project-by-project basis.” In fact the legislation specified patent policy only for the NSF, not for all agency chiefs. Likely influenced by Bush, it authorized the granting of patent rights in a “manner calculated to protect the public interest and the equities,” meaning the intellectual and practical assets, of the contractor.2
At the time, 90 percent of federal research dollars were supplied by defense agencies and the Atomic Energy Commission. But the National Institutes of Health (NIH), the principal agency for medical and health research, was expanding. In 1955 the secretary of its new home department, Health, Education, and Welfare, announced that the NIH would own the patents arising from all the research it sponsored and would license them widely. If an exclusive license was required for the commercial development of an important medical invention, the surgeon general could grant one through a special Institutional Patent Agreement, on the condition that the contractor make the medicine “available to the public on ‘reasonable terms.’”
Advertisement
Zaitchik, absorbed with ownership, does not adequately address the strikingly important questions that from then on increasingly emerged in federal policy for medical patents that the government helped generate: What did “reasonable terms” mean? And just how energetically would the government define and enforce that requirement?
In 1948 Selman Waksman, a medical microbiologist at the New Jersey Agricultural Experiment Station of Rutgers University, and his graduate student Albert Schatz patented a new antibiotic they called streptomycin. It was produced by a soil microbe and had a potent ability to kill infectious bacteria, including a number that were resistant to penicillin. Streptomycin was patentable under existing law because it was a product not of nature but of what amounted to a man-made biological machine, which enabled the production of the antibiotic by placing the microbe in a nutrient soup. Waksman and Schatz assigned their patent to a Rutgers foundation, which licensed it widely as the first antibiotic treatment for tuberculosis.
Stimulated by the discovery, drug companies searched the earth for promising microbes, and in 1952 industry lobbyists secured a revision to US patent law that, contrary to Zaitchik’s account, did not make natural products such as microbes eligible for patents but required that an invention must simply be “nonobvious” rather than, as a court had recently held, the result of a “flash of creative genius.” The new criterion was met by the mechanical process of screening the soil for microbes with antibacterial properties.
In the postwar years the drug industry boomed, fueled by sales not only of dozens of antibiotics but also of hormones, amphetamines, and tranquilizers. Patents enabled huge price markups, generating corporate profit margins “double and often triple those found in other manufacturing sectors,” Zaitchik writes. Many drugmakers began to sell their products under brand names instead of neutral scientific identifiers (for example, Equanil and Miltown for the tranquilizer meprobamate), vastly enlarged their sales forces, and gave representatives generous expense accounts for entertaining doctors. The leading medical journals reaped sizable income from advertisements for branded drugs. In 1955 the AMA, aligning itself more closely with “business and profit,” revised its principles to allow physicians to patent their inventions as long as they made them and the research that gave rise to them accessible. “Empty words,” Zaitchik comments.
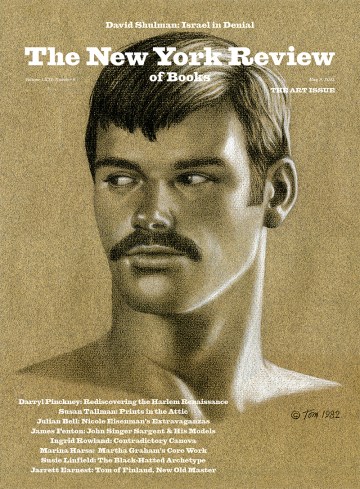
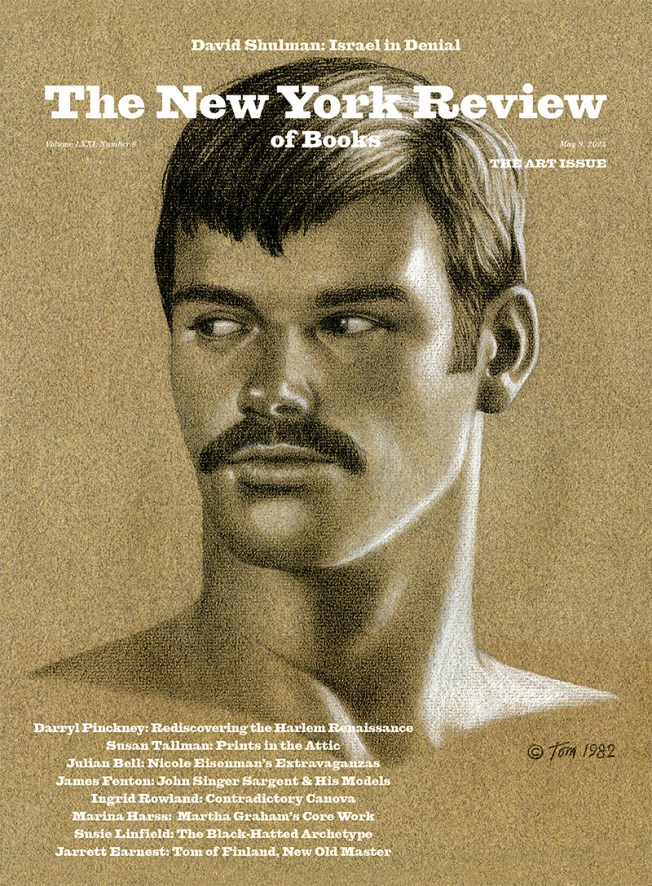
A seeming counter to the trend was Jonas Salk, the physician who developed the first polio vaccine with the support of the National Foundation for Infantile Paralysis (NFIP). Bells rang out across the country when in 1955 a nationwide trial proved it effective. Asked by Edward R. Murrow on his widely watched program See It Now who owned the patent on the vaccine, Salk responded hesitantly, “The people, I would say. There is no patent. Could you patent the sun?”
While Zaitchik acknowledges that Salk was not the first to make a statement of this kind and was by no means indifferent to profiting from his expertise, he neglects to mention that the NFIP had in fact looked into patenting the vaccine. The potential patentability was rooted not in the vaccine itself, which as a dead virus was a product of nature, but in the process used to produce it; however, the foundation’s legal counsel advised that the process was ineligible because it was not novel.3
As patent terms expired, the emerging generic drug industry offered branded medications under scientific names and at much lower prices. The leading brands went to war, declaring generics to be “counterfeits,” unreliable, and dangerous, and lobbying successfully for the passage by 1970 of laws in all fifty states prohibiting pharmacists from dispensing them. (In the mid-1970s, an alliance of the AARP, organized labor, and consumer groups overturned these laws in forty states.)
At the end of 1959 a congressional committee that had been investigating monopoly and price-fixing turned its sights on the prescription drug industry. It was headed by Tennessee senator Estes Kefauver, a reformer in the mold of Kilgore who drew on thousands of pages of testimony to craft a bill that would reform the industry’s patent practices, impose limits on its advertising, and encourage generics. Companies and their medical allies ferociously contested the bill, labeling it, in so many words, socialized pharmacy, an echo of the AMA’s crusade against national health insurance as socialized medicine. In 1962, following the revelation that thalidomide caused birth defects, Congress passed a law that required new drugs to be effective as well as safe but did not take up patent policy.
John F. Kennedy’s administration was attentive to the issues Kefauver sought to address, particularly where they touched on federal funding for medical research, which was ballooning.4 In October 1963 Kennedy issued a memorandum intended to make patenting and licensing practices consistent across federal agencies. Zaitchik emphasizes its instruction that if a federal research contract’s main purpose concerned “public health or public welfare,” the government would “normally” keep the rights to any inventions made under it. However, the memorandum rejected a government-wide policy of “a single presumption of ownership” because it had a “responsibility to foster the fullest exploitation of the inventions for the public benefit.” Agency heads could allow private contractors exclusive rights in “exceptional circumstances,” a phrase that Zaitchik interprets to mean “rare instances” but that was broadly defined to include, in the vein of Vannevar Bush, recognition of the assets contractors brought to the invention and the best means of bringing it into use consistent with safeguarding the public interest.
In August 1971 President Richard Nixon issued his own memorandum for inventions made with federal support. It was friendlier than Kennedy’s to commercialization, yet it authorized the government to “require” a contractor given exclusive rights to grant to others on “reasonable” terms usage of the invention if it was essential for public purposes or was “necessary to fulfill health or safety needs.” Bolstering of the cause of commercialization and calls for federal intervention in the public interest were both harbingers of three dramatic changes in patent policy and law that occurred in 1980.
The first was a broadly bipartisan, joint legislative initiative of the Carter administration and Congress, named after the two senators—Birch Bayh of Indiana and Robert Dole of Kansas—who shepherded the bill to passage in 1980. Intended to inject the energy of new technologies into the American economy, Bayh-Dole was in part a response to the stagflation of the 1970s and the decade’s trade deficits, particularly the increasing Japanese share of the domestic market for automobiles and consumer electronics. It was promoted by corporate executives, patent lawyers, and university managers of intellectual property, who claimed that an “inventions gap” was hindering US competitiveness in international trade and attributed it to a government failure to license university-generated patents to private companies on an exclusive basis. “In general…ideas owned by all will be developed by none,” a leading patent expert told a Senate committee in 1979.5
Bayh-Dole’s major aim was to encourage the commercialization of federally funded university research in collaboration with small business. To that end it reversed the presumption of public ownership of patents arising from federal research grants to universities, instead allowing them to “elect” ownership, including on an exclusive basis, while retaining the government’s right to a cost-free license. Like Nixon’s memorandum, from which it drew concepts and phrasings, Bayh-Dole required patent holders to make the invention’s “benefits…available to the public on reasonable terms.” If they failed to do so, it awarded the government “march-in rights” to take control of their patents for largely the same purposes, including the meeting of “health and safety needs which are not reasonably satisfied by the contractor,” as the Nixon memorandum had addressed.
Zaitchik treats most of the arguments for Bayh-Dole skeptically as covers for a drive by large high-technology corporations to profit from federally supported research. He writes that their target was Kennedy’s memorandum, making no mention of Nixon’s later and more influential version, but he ably presents their neoliberal rationale, provided by the group of academics affiliated with the University of Chicago’s program in law and economics, that regulation dampened innovation.
In attributing Bayh-Dole to the Chicago school’s influence on policymaking, Zaitchik relegates to insignificance the wide array of interests and opinion makers that promoted the legislation. He writes that advocates of big business accepted its spinout limitation to small business as a matter of political expediency, expecting that it would eventually be lifted to allow large corporations to partake of the government’s largesse. If that was their expectation—Zaitchik offers no smoking-gun evidence that it was—they were correct. In 1983 President Ronald Reagan removed the limitation by executive order.
Oddly, in a book about the business of drugs, Zaitchik pays no more than casual attention to the budding biotechnology industry. Major hopes rested on it—and on personal computing—to reverse the trade deficit. Biotech drew its intellectual capital from academic innovations in molecular genetics. Universities licensed their patents to firms, many of them founded by their professors, often on an exclusive basis. These start-ups, some of them launched in basements and garages, had a stake in Bayh-Dole, too. The legislation was far more than a small business stalking horse for the patent aspirations of large corporations.
The Carter administration initiated the second part of the trifecta by urging Congress to overhaul how the federal courts dealt with patent suits. At the time, suits could be filed in dozens of federal district courts and carried forward in eleven different federal appeals courts. Congress streamlined the system by establishing a single federal appeals court in Washington to hear them all.6
The biotechnology industry had a substantial interest in the third major development of 1980: the Supreme Court’s ruling in the patent case Diamond v. Chakrabarty. Contrary to Zaitchik, the case did not concern the “modified genes” in an altered bacterium but centered on the bacterium itself, which Ananda Chakrabarty, a microbiologist at General Electric, had altered to metabolize oil into protein. The core issue was whether a living organism could be patented. Commissioner of Patents Sidney A. Diamond held that it could not. Multiple amicus briefs, including from university patent administrators and the new firm Genentech, contended it could.
The Court in effect awarded Chakrabarty his patent, ruling by a vote of 5–4 that his modified bacterium qualified for a patent and thus establishing the doctrine that whether an invention was alive was irrelevant to its patent eligibility. This immediately helped the medical wing of the biotech industry by allowing patents on the bacteria it was genetically engineering to produce vital substances such as insulin and blood-clotting agents.7
From the 1980s onward the drug industry expanded enormously, especially after the passage of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, which authorized Medicare coverage of prescription drugs to senior outpatients, and the federal government’s eager investment in biomedicine. Profits continued to rise even after 1984, when Congress bolstered competition from the generics industry with the Hatch-Waxman Act. But while generics offered much cheaper versions of drugs whose patents had expired, the act, granting “data exclusivity” to branded drugs for five to seven years, in effect extended their patent life beyond the statutory term, which was then seventeen years. (It was raised to twenty in 1995.) And by patenting slightly modified versions of a drug—one of several ploys to game the system—various companies managed de facto to extend the patent term still further, a process called evergreening. As in the recent notorious case of insulin, they tended to sell the protected drugs at prices unaffordable for many consumers, maintaining, without specific supporting data, that they required sizable revenues to offset the costs of development, including research, clinical trials, and frequent failures.
In the early 1980s the interpretation of the public interest and reasonable-terms features of Bayh-Dole was up for grabs. Federal agencies might have taken them to mean that they possessed the authority to exercise march-in rights to rein in prices, at least of drugs developed with federal support. But heads of agencies—which for prescription drugs meant mainly the Department of Health and Human Services and the NIH within it—were far more absorbed with making the drugs available for public use, mainly by commercialization, than with holding private contractors to account. The costs to patients could be enormous, as when in the mid-1980s the National Cancer Institute (NCI) stood by while an American subsidiary of the British pharmaceutical company Burroughs Wellcome patented the drug AZT, the first treatment for AIDS, and when it went on the market in 1987 charged as much as $10,000 (almost $20,000 today) for a year’s supply.
Zaitchik misguidedly presents the matter as a number of congressmen and AIDS activists saw it at the time, just after the cause of AIDS had been identified as a virus (HIV): the NCI had “invented and rediscovered the drug,” and so could have claimed ownership and licensed it for production and sale at a much lower price. But while AZT had been developed in 1964 under an NCI grant, it had failed as an anticancer drug and come into the public domain. More important, it was not the NCI that recognized AZT as a likely agent against HIV but Burroughs Wellcome, whose scientists had observed that the drug adversely affected mouse viruses similar to HIV. At the company’s request, the NCI tested AZT and was the first to find that it displayed effectiveness against live HIV.
Still, even though the NCI didn’t rediscover AZT, it could have bargained for coinventor status when it agreed to perform the tests, claiming that its cooperation subjected the drug to the public interest provisions in Bayh-Dole or, at the very least, that it enabled the NCI to obtain a commitment from Burroughs Wellcome to sell the drug at a reasonable price. “We didn’t pick up fast enough on the cost issue,” Samuel Broder, the initiator and a high-ranking NCI oncologist who had run its testing program, told a reporter. By late 1987, under public pressure, the company had reduced the price of a year’s supply to $8,000—but it continued to earn tens of millions of dollars (by 1991 cumulative worldwide sales would top $1 billion) while untold numbers of AIDS patients were struggling to pay for it. Broder later said privately that he had been naive.8
Skyrocketing drug prices in the years following prompted a growing number of public policy advocates, pointing to Bayh-Dole’s reasonable-terms clause, to call on the government to exercise its march-in power to ensure reasonable prices for drugs developed with federal support. In 2002, however, Bayh, who at the time was part of a Washington law firm whose clients included pharmaceutical companies, and Dole, then extolling Viagra on television, contended that their legislation had never been intended to control drug prices. Between 1997 and 2016, the NIH received six petitions requesting that it exercise march-in rights over six different drugs. It declined them all, arguing, among other reasons, that “the issue of drug pricing” belonged to Congress.
None of the principals were naive in May 2020, when President Donald Trump announced Operation Warp Speed. The initiative, Zaitchik writes, “let the companies maintain controlling patent rights [on the vaccines and the processes for producing them] without any corresponding obligation on pricing or technology transfer to the rest of the world.” The legality of such transfers was shadowed by the international Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS), concluded in 1994 in conjunction with the establishment of the World Trade Organization.
Engineered by the developed countries of the Global North, most of which permitted drug patenting, TRIPS was intended to halt what they saw as piracy by less developed countries. Countries in the Global South lacking domestic capacity for pharmaceutical innovation justified the practice of appropriating the North’s drugs on the grounds that public health should take precedence over commercial interests. India, a leader in the South’s defiance, had even prohibited pharmaceutical patents in 1970. TRIPS countered this resistance by requiring adherents to the agreement to honor the patents issued by other countries and to establish suitable patent regimes of their own.
More than 120 states signed on to the WTO and TRIPS, those from the South brought in by the prospect of increased trade and threats of economic retaliation if they stayed out. Patent restrictions had denied them affordable AIDS drugs, and, adamantly unwilling to repeat that experience, between 2001 and 2003 the South pushed through a modification of the agreement that formally allowed “flexibility” in its rules, notably the imposition of compulsory licensing for health emergencies. But in practice, according to Zaitchik, such latitude fell victim to northern intimidation and bullying: the North coerced the South to conform to TRIPS, governments threatened to raise tariffs on the South’s exports, and a multinational pharma lawsuit prevented South Africa from importing and producing low-cost drugs. In 2006 the economist Joseph Stiglitz, a member of the Council of Economic Advisers when TRIPS was created, said the agreement likely meant a “death warrant for thousands of people in the poorest countries of the world.”
To the Trump administration, TRIPS was sacrosanct. Activists in the South and their supporters in the North called for an international pooling of Covid data, collaboration in the development of pharmaceutical remedies, and a temporary waiver of TRIPS during the pandemic for Covid vaccines and related drugs. Trump’s secretary of health and human services, Alex Azar—a former president of the US division of Eli Lilly—claimed that such measures might “negatively affect countries’ abilities to incentivize new drug development.” Bill Gates, who enjoyed a sage-like influence on international drug policy not least because of his munificent philanthropic assistance to the battle against AIDS, forcefully opposed patent waivers and did his best to block any dilution of the TRIPS patent regime.
Northern demand for vaccines took up most of the supply in the first year of their availability, which made urgent the South’s ability to manufacture its own supply. In May 2021 the Biden administration announced that it would support an emergency waiver of the patent rights on Covid medications for the benefit of populations elsewhere in the world. The Bill and Melinda Gates Foundation, under mounting public pressure, conceded that “no barriers should stand in the way of equitable access to vaccines, including intellectual property.”
A week after the White House’s announcement, Stéphane Bancel, the CEO of Moderna, told financial analysts that he “didn’t lose a minute of sleep over the news.” As he well knew, and as Zaitchik rightly points out, patents are only one means of maintaining a medical monopoly. Another is to keep hidden, as trade secrets, the detailed data, expertise, and technologies necessary to produce a medication. Patent law does not require the disclosure of such knowledge, and US law (since the Tariff Act of 1930) and TRIPS both protect trade secrets indefinitely. Their misappropriation for commerce or espionage was made a federal crime in 1996, and they have emerged in recent years as a means to suppress the production of generics in the US and duplicates of lifesaving drugs in the Global South. According to the UN, as of July only one in three people in low-income countries have been vaccinated against Covid-19.
Beginning in late 2021 Covid vaccines were increasingly obtainable in the US under Medicare, Medicaid, Obamacare, and private insurance at little to no cost, and boosters were even easier to get after Biden established federal subsidies for them. In the past year, federal enforcement of access to a wider range of medications at reasonable prices has gained national traction. Reformers have called for Bayh-Dole to be updated so that march-in rights are practically workable and pricing is included in the definition of “reasonable terms.” With the passage of the Inflation Reduction Act in August 2022, the Biden administration overcame fierce industry opposition to give the secretary of health and human services the authority to negotiate price reductions in high-cost prescription drugs available through Medicare, starting with ten drugs in 2026, fifteen more in each of the next two years, and twenty every year thereafter. The act also for the first time capped out-of-pocket spending on drugs by Medicare recipients at $2,000 a year. But Moderna’s huge intended price increase prompted Senator Bernie Sanders to urge much prompter action. With sardonic fury, he asked of Bancel on the Senate floor:
How is the CEO of this company thanking the taxpayers of this country who are responsible for making him and his colleagues incredibly rich? He is thanking them by proposing to quadruple the price.
Zaitchik closes his book with a prosecutorial assessment:
Covid-19 has pushed the issues around monopoly, intellectual property, and technology transfer…closer to their rightful place as burning public questions of global security, health, and justice…. By the standards of any civilization that views its medicines as crowning achievements, the regime that prices them beyond reach and restricts the knowledge to make them must be, and has been, ruled a failure.
Not a failure, but rather, in an era when health care is widely held to be a human right, a perversion of the system’s necessary purposes: not only to enable the drug industry to produce a powerful and profitable pharmacopoeia but to ensure that those products are equitably available to consumers at reasonable prices. Pharma continues to resist its latter obligation; several major drug companies as well as the industry’s principal trade group have filed suits against Medicare’s new price-negotiating authority. In the face of the industry’s enormous power, resolute federal intervention is essential. In mid-February, the same day that Sanders announced a Senate hearing on Moderna’s pricing, the company backtracked: “Everyone in the US will have access to Moderna’s Covid-19 vaccine regardless of their ability to pay.”
-
1
For more on this subject, see my “Why Is Medicine So Expensive?,” The New York Review, February 21, 2019. ↩
-
2
The primary reason for the delay in the legislation was not patents but Bush’s insistence on insulating the NSF administratively from presidential authority. In 1947 the conservative 80th Congress approved a bill with such an arrangement, but Truman vetoed it. Zaitchik, ignoring Truman’s veto, declares that Truman “betrayed” the New Deal commitment to public science under public control. ↩
-
3
See Jane S. Smith, Patenting the Sun: Polio and the Salk Vaccine (William Morrow, 1990). Disease-oriented philanthropies have come to exert sizable influence over research on their targets and the patent rights to the outcomes, a subject that awaits systematic analysis. ↩
-
4
By 1962 the NIH budget had reached $495 million, almost quadruple that of 1957. ↩
-
5
The rate of commercialization of an invention was almost twice as high (23.8 percent) when the contractor held title to the patent than when the government retained the title (13.3 percent). See Rachel Sachs, “The New Model of Interest Group Representation in Patent Law,” Yale Journal of Law & Technology, Vol. 16 (Spring 2014). ↩
-
6
According to Zaitchik, the reform arose from industry’s dissatisfaction that the decentralized system allowed too many New Deal–minded judges to reject patent claims. He may be right, but the establishment of the single appeals court answered several problems of the prior structure, including its allowance of what an informed observer called “forum shopping,” the selection of a jurisdiction where the plaintiff in an infringement suit might hope for a favorable outcome, as well as variant, conflicting standards of patentability from different courts. ↩
-
7
The decision also laid the foundation for legal rulings in the 1980s that enabled the patenting of any plant and of any animal other than a human being, both of consequence for biomedical experimentation and agricultural biotechnology. ↩
-
8
See Peter S. Arno and Karyn L. Feiden, Against the Odds: The Story of AIDS Drug Development, Politics and Profits (HarperCollins, 1992). NCI later wanted to sue for rights as a coinventor in the Burroughs Wellcome patents but was unable to gain support from President George H.W. Bush’s Justice Department. In the early 1990s two generic pharmaceutical firms filed suit against the company, contending that its patents should be invalidated because they did not include as coinventors the NCI scientists who had demonstrated AZT’s activity against HIV. The new patent appeals court in Washington ruled unanimously in Burroughs Wellcome’s favor on the essential AZT patents. The court acknowledged that NCI had brought skill, experience, and an ability to interpret the data to its testing but credited Burroughs Wellcome as the sole inventor, because before sending it to Broder the company had conceived of AZT as a drug against HIV in substantively specific terms. ↩